According to the Ministry of Healthcare of the Russian Federation, over the last 15 years the stillbirth rate (ICD-10 codes: Q00-Q99, P05, P08, P20, P35, P37, P39, P 50, P52, P55, P56, P60, P61, P70, P75, P77, P83, P95) has been quite stable: 2005 — 5.68, 2010 — 4.62, 2015 — 5.87, 2018 — 5.51 per 1000 babies born alive and dead [1]. Whereby death before parturition was observed in 89 % of cases [2]. According to foreign authors the stillbirth rate in the USA is approximately estimated as 3.05 per 1000 births [3]. Although the Russian Federation’s stillbirth rate is practically twice as high as that of the USA, there aren‘t any Russian clinical guidelines. Since medical assistance to patients with stillbirth includes anaesthesia, it is necessary to develop agreed interdisciplinary documents. This study was initiated to determine the degree of consensus on this issue among the experts in obstetrics and gynecology, anaesthesiology, and resuscitation. This work was supported by the Russian Obstetrical Anesthesiologists and Intensivists Association (ROAIA).
The Objective of this study was to analyze the results of a survey of obstetricians-gynecologists and intensivists.
We have developed a questionnaire, which consisted of 23 questions in Russian. It was reviewed by the Research Committee of ROAIA and tested to assess the understanding of the target audience in the cohort of 20 intensivists and 20 obstetricians-gynecologists. We have considered all the received comments and proposals. The final survey contained the following questions: specialty and length of service, sex, their region of residence, experience in helping patients with stillbirth, the difficulty of communication with such patients, attitude to deep sedation of a mother giving birth to a dead fetus, opinion on the impact of contact of the mother and her dead fetus on the woman’s mental status, opinion on the best method of stillbirth analgesia, implementation of a patient’s desires during labour, the attitude of medical personnel to the tactics of managing stillbirths in their medical institution, postpartum period problems and determining the conditions of stay for patients with stillbirth, provision of psychological support to patients, the satisfaction of women and medical personnel with the childbirth care services in this situation, the need for developing clinical guidelines and trainings devoted to assisting women with stillbirth. The structure of the survey also allowed to prepare a semi-structured interview for detecting factors that influence decision-making process.
We published the survey on Google Forms online resource (https://forms.gle/rEnvMbkuUAmbGHXd6). The links to this survey were available on closed theme-based online resources for intensivists, obstetricians-gynecologists, and other experts working in childbirth care institutions. The survey was also sent by email to the leading research centers of obstetrics and gynecology in the Russian Federation, the Ukraine, Republic of Moldova, Republic of Tajikistan, Republic of Uzbekistan, Republic of Belarus, Republic of Azerbaijan, Republic of Estonia, Republic of Latvia, Republic of Lithuania, Republic of Armenia and Georgia. The respondents were offered to take part in the online survey from 28 June 2019 until 29 February 2020. The questionnaires were filled in anonymously and voluntarily. We have checked the uniqueness of IP address to make sure users wouldn’t duplicate their answers. This web survey was developed and published on e-resources according to the current guidelines [4–6].
Every question of the questionnaire allowed us to prepare a rating of answers characterising a factor influencing the decision on managing pregnant women with stillbirth during labour and in postpartum period. The rating represents a distribution of a relative frequency (in percentage points) of all supposed answers to given questions. The stated distribution of relative frequencies was calculated inside groups of experts: intensivists and obstetricians-gynecologists. We used chi-square test and Fisher’s exact test to check the hypothesis of statistical significance of difference of the stated ratings between expert groups . The input data were accumulated in the format of an Excel chart (Microsoft Excel 97–2003). All calculations and statistical analysis of data were carried out using SPSS Statistics (version 17.0, update dated 28.07.2019). The level of significance of various frequency distributions of ratings was assumed to be 0.05.
A total of 369 Russian-speaking doctors, intensivists, and obstetricians-gynecologists from more than 30 Russian regions and 11 CIS and non-CIS countries took part in the survey. 63.4 % (n = 234) of the participants of the survey were intensivists and 36.6 % (n = 135) were obstetricians-gynecologists. The survey has sparked the most interest among medical personnel with over 20 years of service (n = 124; 34 %). Whereby distribution of respondents by the length of service was statistically different in two groups (p = 0.001). The compared groups were also statistically different by gender index (p < 0.0001). Intensivists were predominantly male (n = 138; 59 %), whereas most part of obstetricians-gynecologists were female (n = 102; 76 %) (Tab. 1).
Table 1. Description of respondents
| Specialty | Length of service (in years) |
Sex | Total | |
|---|---|---|---|---|
| Men | Women | |||
| Intensivists | < 5 | 18 (13.0/4,9)* | 16 (16.7/4.3) | 34 (14.5/9.2) |
| 5–10 | 21 (15.2/5.7) | 24 (25.0/6.5) | 45(19.2/12.2) | |
| 10–20 | 42 (30.4/11.4) | 26 (27.0/7.0) | 68 (29.1/18.4) | |
| > 20 | 57 (41.4/15.5) | 30 (31.3/8.1) | 87 (37.2/23.6) | |
| Total | 138 (59.0/37.4) | 96 (41.0/26) | 234 (100.0/63.4) | |
| Obstetricians-gynecologists | < 5 | 9 (27.3/2.4) | 29 (28.4/7.9) | 38 (28.1/10.3) |
| 5–10 | 7 (21.2/1.9) | 28 (27.5/7.6) | 35 (25.9/9.5) | |
| 10–20 | 8 (24.2/2.2) | 17 (16.6/4.6) | 25 (18.5/6.8) | |
| > 20 | 9 (27.3/2.4) | 28 (27.5/7.6) | 37 (27.4/10) | |
| Total | 33 (24.4/8.9) | 102 (75.6/27.6) | 135 (100.0/36.6) | |
| TOTAL number of doctors | – | – | 369 (100.0) | |
* The results are represented in the form of n (% of the number of respondents in the group / % of the total number of respondents).
The data analysis has shown that the practical experience of working with stillbirth was statistically different among different experts. Obstetricians-gynecologists (n = 104; 77 %) encountered stillbirths 12 % (p = 0.028) more often than intensivists (n = 152; 65 %).
In spite of having less experience of working with stillbirths most intensivists (n = 133; 57 %) considered it easy for them to build relationships with this category of patients. Obstetricians-gynecologists had no difficulties in communicating with patients with stillbirths in 67 % (n = 90) of cases. However, 1/3 of experts of both specialties (intensivists [n = 65; 28 %] and obstetricians-gynecologists [n = 38; 28.5 %]) experienced problems in communicating with this group of women. The response ratings had a statistically significant difference between the compared groups of experts: p = 0.025.
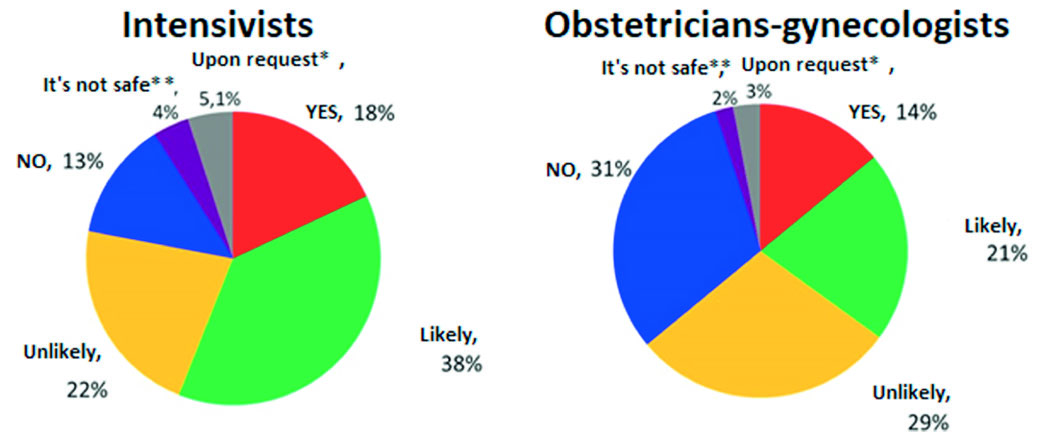
The need to turn off the mother’s consciousness at the time of giving birth to a dead fetus caused the greatest disagreement. The ratings of answers to this question showed a significant difference in opinions between experts in different fields (p = 0.0001). More than half (n = 131; 56 %) of intensivists were in favour of turning off the mother’s consciousness at the time of giving birth to a still fetus. Less than 13 % (n = 30) of doctors of this specialty are absolutely against this opinion. 35 % (n = 47) of obstetricians-gynecologists were in favour of turning off the mother’s consciousness. Most (n = 81; 60 %) respondents from this group preferred to refuse from deep sedation of the mother (Fig. 1).
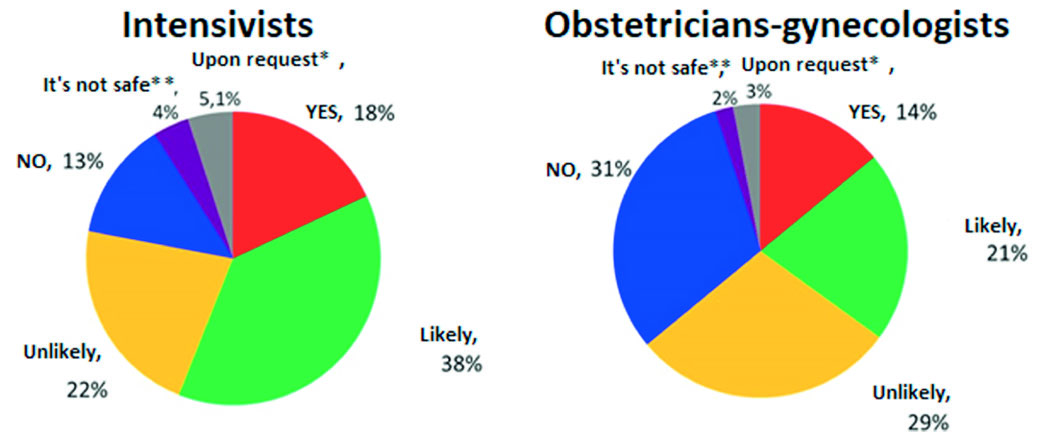
Fig. 1. “Do you consider it necessary to carry out deep sedation of the mother at the time of the birth of the still fetus?”
* If so desired by the patient.
** I consider sedation necessary, but I do not use it due to the lack of conditions for its safe administration.
The question about the impact of visual and tactile contact of a mother and her dead fetus on the psychoemotional state of the woman has also become quite controversial. Only 1/5 of obstetricians-gynecologists (n = 31; 23 %) and 1/10 of intensivists (n = 20; 9 %) think that the contact of a mother and her dead baby has a positive impact on her. Whereby almost 1/2 of intensivists (n = 110; 47 %) and 1/3 of obstetricians-gynecologists (n = 46; 33 %) consider this impact to be negative, and 1/3 of respondents in both groups (intensivists [n = 63; 27 %] and obstetricians-gynecologists [n = 40; 30 %]) insist that this measure has an absolutely negative effect. Thus, the frequency distribution of answers to this question was significantly different between the respondents of these two groups: р = 0.002 (Fig. 2).
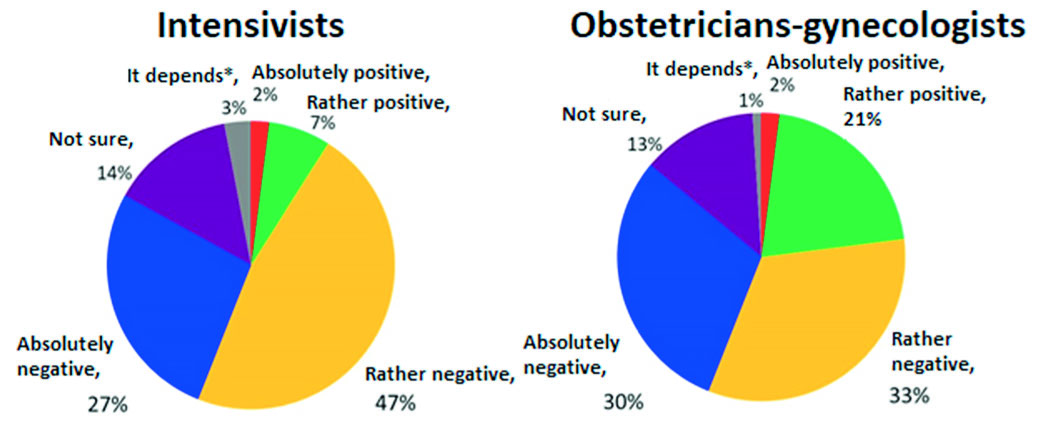
Fig. 2. “Do you think visual and tactile contact between a mother and a stillborn child has a positive impact on the psychological and emotional state of a woman in the long term?”
* Depending on individual characteristics and desires of the patient.
Intensivists and obstetricians-gynecologists have been unanimous as per the best method of analgesia. Both groups of experts (intensivists [n = 145; 62 %] and obstetricians-gynecologists [n = 71; 53 %]) preferred epidural analgesia in more than half of the cases (57.5 %); however, there is a significant difference regarding all other variants (narcotic analgesics, no analgesia, turning off the mother’s consciousness at the time of giving birth to a dead fetus). On the whole, the difference of ratings on this issue among experts has not reached statistical significance, but it has come close to its threshold value: р = 0.056.
58 % (n = 136) of intensivists and 48 % (n = 65) of obstetricians-gynecologists ask the patient about her desire to stay conscious when giving birth to a dead fetus. Answers to this question have revealed no differences between the groups of experts (р = 0.117).
The respondents have also shown unanimity regarding the optimal tactics of analgesia provision during birth of a dead fetus in their medical institutions. Thus, 59.5 % (n = 210) of respondents think that the method of anesthesia used in their medical institution is optimal, 9 % (n = 33) do not think so, 31.5 % (n = 116) say that their medical institutions have no unified anesthesia approaches for birth of a dead fetus. The answers to this question have not revealed the differences between the groups of experts (р = 0.276).
More than half of intensivists (n = 131; 56 %) and obstetricians-gynecologists (n = 78; 58 %) think that psychological disorders are the most frequent issue the patients with stillbirth can suffer from. However, the frequencies of specifying other problems were significantly and statistically different (intensivists mentioned haemostasis pathology and a combination of problems, whereas obstetricians-gynecologists pointed out to obstetric complications), thus, on the whole, the intergroup difference of ratings also reaches statistical significance: р = 0.003.
The opinion regarding the best place of stay of a patient before being discharged from an in-patient facility is also quite consistent. Most respondents (n = 244; 66 %) think that for the woman it is better to stay in an isolated ward, 23 % (n = 85) of respondents hospitalise the patient into a gynaecological department, 7 % (n = 25) place patients of this group in the wards with other maternity patients and 4 % (n = 15) mention the opportunity of establishing a specialised ward (stay with relatives or a psychologist). Thus, there is no significant difference in the ratings between the experts of the compared groups: р = 0.654.
Among intensivists 50 % (n = 117) of respondents think that postpartum sedation is not used in their medical institution, 37 % (n = 86) have stated that they prescribe benzodiazepines, 12 % (n = 28) opt for botanicals, and 1 % (n = 3) resolve this issue with every patient on a case-by-case basis. The number of obstetricians-gynecologists prescribing postpartum sedation was significantly higher (n = 95; 70 %). Among them 58 % (n = 56) of respondents use benzodiazepines, 38 % (n = 36) apply botanicals, 4 % (n = 3) resolve this issue with every patient on a case-by-case basis. Frequency distributions of answers to this question were significantly different between the groups of experts (р <0.0001).
The data of the national study show the absence of a full-fledged medical and psychological support in one of three institutions of the country (n = 127; 34 %). One in ten (n = 36; 10 %) respondents was not interested in the provision of professional psychological care in the in-patient facility. However, more than half of these respondents (n = 214; 58 %) have mentioned before that it is easy for them to build up supportive communication and show care for patients. In the institutions that rendered psychological support most of the respondents (n = 136; 37 %) thought that the psychological care was provided to this group of patients in a complete volume, and one in five respondents (n = 70; 19 %) stated that the volume was incomplete. The answers to this question have brought out no differences between these groups of experts (р = 0.130).
Regarding the satisfaction with the quality of medical care among patients with stillbirth the compared groups of medical personnel were also unanimous. On the average, 71.5 % (n = 264) of respondents think that the patients are satisfied with the medical assistance rendered to them. The ratings of answers to this question do not have statistically significant differences between two groups of respondents: р = 0.071. It is worth mentioning that this judgement may not be objective, because it mostly reflects the subjective opinion of the experts. We considered that one third of experts (n = 86; 32 %) who positively responded to this question did not take into account the patient’s opinion about selecting the method of analgesia and did not possess the information about the course of her postpartum period. The incomplete correspondence of answers with the following question shows this as well.
Most respondents from both groups of comparison (n = 250; 67.5 %) think that patients rarely submit complains and claims on the quality of medical assistance rendered to them, and 16 % (n = 59) of respondents have never faced patient dissatisfaction. However, 13.5 % (n = 49) of respondents frequently face complains and claims of this group of patients, and 3 % (n = 11) almost always face them. The ratings of answers to this question do not have statistically significant differences between 2 groups of respondents: р = 0.963.
The question about the doctor’s satisfaction with the rendered assistance showed ratings that were different among the experts (р < 0.0001). Almost half of the respondents of both groups (intensivists [n = 115; 49 %] and obstetricians-gynecologists [n = 57; 42 %]) selected the answer “rather no”. And the share of intensivists who gave a clear positive answer (n = 47; 20 %) was twice less than that of obstetricians-gynecologists (n = 54; 40 %). The share of respondents answering “rather no” among intensivists (n = 40; 17 %) was almost 6 times higher compared with obstetricians-gynecologists (n = 4; 3 %) (Fig. 3).
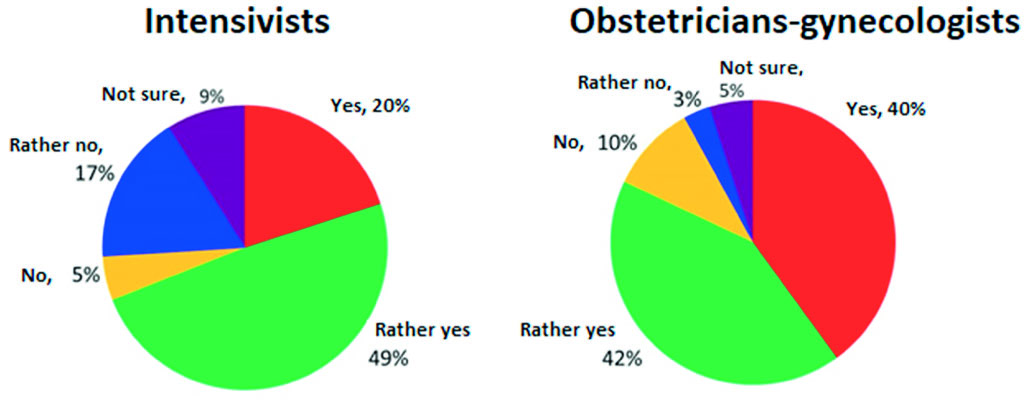
Fig. 3. “Are you satisfied with the quality of medical care for patients with stillbirth in your hospital?”
The ratings of answers to the question about the need for developing clinical guidelines on the studied problem do not have a statistically significant difference between the groups of respondents (р = 0.071). Obstetricians-gynecologists are more confident in the need of such guidelines (75 % [n = 101] — “definitely yes” and almost 20 % [n = 26] — “rather yes than no”), than intensivists (64 % [n = 150] — “definitely yes” and almost 22 % [n = 51] — “rather yes than no”). Only 6 % (n = 8) of obstetricians-gynecologists and 14 % (n = 33) of intensivists gave a negative answer to this question.
The question about the need of trainings/workshops has shown bigger differences between the experts of different profiles (р = 0.011). Slightly less than 1/5 (n = 40; 17 %) of all respondents among intensivists are rather or definitely negative regarding this idea, whereas only 1/20 (n = 7; 5 %) among obstetricians answered this way.
The received data clearly show disagreement between intensivists and obstetricians-gynecologists regarding the need to turn off the consciousness of a mother giving birth to a dead fetus, the impact of visual and tactile contact of a mother and her dead fetus on her psychoemotional state in the long-term, the need of sedation in postpartum period. Obstetricians-gynecologists are more experienced in working with stillbirth than intensivists. However, intensivists’ length of service is significantly above that of obstetricians-gynecologists (see Tab. 1).
The difference between the length of service and experience of working with stillbirth is most likely related to managing childbirth without intensivists.
Intensivists find it as easy to communicate with this group of patients as obstetricians-gynecologists. This can stem from longer service of intensivists, gender heterogeneity of the groups with the prevalence of men’s standpoint among intensivists and personal characteristics that are more typical for people who chose anesthesiology and resuscitation as their specialty.
The adherence of intensivists to turning off the mother’s consciousness at the time of giving birth to a dead fetus, unlike obstetricians-gynecologists, stem from many factors. Probably, the main role in this process is played by intensivists’ strong belief (almost 90 %) in the negative impact of contact between the mother and her stillborn baby. When discussing possible reasons of a disagreement that significant, it’s necessary to consider the results of semi-structured interviews’ analysis. About 8 % (n = 10) of obstetricians-gynecologists stated that they are afraid of patients’ lawsuits resulting from patients’ mistrust to the personnel and prefer that the woman witnessed the stillbirth in spite of a possible psychological trauma. However, 23 % (n = 31) of all obstetricians-gynecologists who were female consider the contact of mother and fetus necessary, probably judging by the experience of their own maternity. Male intensivists in 24 % (n = 56) of cases explained the need of a deep sedation of the mother by humane treatment of the bereaved woman. The studies conducted in the Russian Federation demonstrate prevailing negative attitude of medical personnel to a woman’s staying conscious when giving birth to a dead fetus as well as to her contact with the dead baby [7]. Foreign studies conducted in other developed countries demonstrate decreased risk of mental disturbances and their severity in postpartum period for women with stillbirth who found themselves in the environment where they could see their stillborn baby, hold it, say goodbye to it and comprehend what has happened [8–11].
It is worth mentioning that one in five experts is guided by their own opinion rather than the patient’s desire when selecting the tactics of managing childbirth. However, it is necessary to specify that most respondents thought that it is easy for them to build up supportive relationship with a patient. One cannot but mention the subjective nature of the experts’ opinions about their communicative abilities, because according to the literature, communication with families that experienced perinatal loss is not always built up by doctors in the appropriate manner [7, 12, 13].
Different opinions regarding postpartum sedation of patients with stillbirth can be explained by the fact that obstetricians-gynecologists take more active part in managing postpartum patients than intensivists.
A possible reason for lesser satisfaction of intensivists when assisting this group of patients and their rejection of professional development can be burnout syndrome related to their longer service.
Although many publications devoted to fetus death are present in Russian and foreign literature, all of them cover the issues of forecast, estimation of reasons for stillbirth and demographic patterns of this pathology leaving out the aspects of managing childbirth with the dead fetus and discussing the patients’ desires.
Since the groups of respondents had statistically significant difference both in terms of the length of service and gender composition, significant mismatch of ratings for approximately half of the survey’s questions cannot be explained by different medical specialties alone. However, the questions having the most different ratings illustrate the existence of many unsolved problems and require joint development of agreed documents on the optimal management of pregnant women with stillbirth.
Developing of new clinical guidelines requires possessing own data, including the ones that consider the national mentality and the opinion of the patients that have experienced a perinatal loss. This will be discussed in our further studies.
Conflict of Interest. The authors state that the conflict of interest is absent.
Contribution of Authors. Mysovskaya Y.S., Marshalov D.V., Shifman E.M., Shindyapina N.V., Ioscovich A.: developing the article’s concept, collecting and analyzing practical evidence, writing and editing the article’s text, checking and approving the article’s text.