PICS (Post Intensive Care Syndrome) is a complex of somatic, neurologic, and social-psychological complications that limits or reduces the quality of life. It develops in patients after the treatment at the Department of Anesthesiology, Intensive Care (ICU) that lasted more than 72 hours and requires rehabilitation [1–3].
PICs-P (Post Intensive Care Syndrome — Pediatrics) is a Post Intensive Care Syndrome that develops in children and the patient’s infant or adolescent family members [4].
Therapeutic Immobilization (TI) is a condition of an artificially limited motor and cognitive activity of a patient caused by analgosedation. It aims to reduce metabolic needs during the treatment of emergency conditions in the ICU.
Therapeutic Deafferentation (TD) is an artificial reduction of perception (sensory organs) and proprioception (internal organs) via drug-induced analgosedation.
Bed-Rest is an approach to a patient’s positioning, which is applied as an immobilization component in the acute period of the disease or early postoperative period. It is used in ICU conditions as a method of therapeutic immobilization.
Learned Non-Use is a mechanism of conditional and unconditional reflex impairment associated with sensory isolation and artificial limitation of the patient’s motor activity during the period of immobilization. It leads to the formation of persistent multiple organ dysfunction manifested as PICS syndrome (ICU-acquired weakness, dysphagia, decrease in the gravitational gradient (GG), and cognitive-sensory dissonance).
ICUAW is an ICU-acquired weakness that develops in patients during immobilization. It is a complex of neuro-muscular impairments (polyneuropathy and/or myopathy) that are clinically manifested as general muscular weakness and peripheral limb paresis. The term Respiratory ICU-acquired weakness should be used for long-term ICU patients with difficulties in withdrawing from continuous mandatory ventilation [5].
Dysphagia is a clinical symptom of swallowing impairment, which causes discomfort or difficulty in passing food from the mouth to the stomach. It develops because of the failure of food passage from the mouth to the stomach. The term post-extubation dysphagia (PED) or ICU-acquired dysphagia is used for patients with tracheoesophageal separation (endotracheal cannula and nasogastric tube) with signs of dysphagia.
Cognitive-sensory dissonance is a condition of space, time, and personality disorientation caused by therapeutic deafferentation.
ICU-acquired dyssomnia is a sleeping disorder in ICU patients associated with 24-hour special technological conditions (constant illumination and noise).
Rehabilitation Potential (for ICU patients) is a possibility of the preservation of the patient’s premorbid socialization status evaluated by the Rehabilitation Routing Scale (RRS).
ICU Rehabilitation (RehabICU) is a complex therapeutic strategy targeted to prevent and treat initial PICS manifestations in ICU patients performed by a multidisciplinary rehabilitation team (MDRT) at the Early Rehabilitation Unit (ERU).
Multidisciplinary Rehabilitation Team (MDRT) is a team of specialists that cooperate to provide a complex of therapeutic and diagnostic measures on the prevention and treatment of PICS according to the Guidelines on medical rehabilitation [5].
Gravitational Gradient (GG) is a maximal lifting angle of a patient that does not lead to the development of orthostatic insufficiency. The normal value corresponds to 90°, i.e. physiological condition of the upright position.
Orthostatic Insufficiency (OI) is a condition of the impaired mechanism of a vegetative control of GG that is manifested as a loss of hemodynamic homeostasis when a patient changes their position from a horizontal to vertical one.
Verticalization (VT) is a diagnostic and training procedure of controlled body verticalization for the evaluation of GG and orthostatic insufficiency. As a component of mobilization, verticalization targets the prevention and treatment of GG impairments in patients that had bed-rest for over 24 hours, regardless of the mental and motor status of the patient.
Positioning (PT) or Postural Correction is a therapeutic and preventive procedure. The patient is helped to take the optimal positions that contribute to the prevention of complications after immobilization (bed-rest or premobilization period of a critical condition) and restoration of the mechanisms of GG and locomotion maintenance, in particular, upright posture. Positioning is based on the method of management of postural muscular-tonic reflexes involving ontogenetic mechanisms of balance maintenance. Depending on the application, positioning is divided into vertical and horizontal.
Vertical positioning (antigravity) (VP) is a method of patient’s vertical positioning for the maintenance or (and) restoration of normal GG and treatment of orthostatic insufficiency. VP aims to adapt the patient to the GG achieved during verticalization maneuvers. As a rehabilitation measure, VP provides a gradual increase in the time of being at each point of GG achieved during verticalization. It should become as close as possible to the target positioning (6–8 hours in the sitting position with periods of returning to the horizontal resting position). It should be noted that VP is associated with an increase in energy demands, which limits the application of this method in the acute period of critical condition when the strategy of metabolic rest is applied.
Non-vertical (pressure-relieving) horizontal positioning (NVP) is a periodic change in the patient’s position in a horizontal plane that substitutes the lack of patient’s movements because of pathological (paresis, plegia) or therapeutic (general anesthesia, analgosedation, myorelaxant application) immobilization. NVP aims to prevent the formation of abnormal postural sets and disturbances in the microcirculation in the points of pressure on the skin (shoulder blade, hind-head, sacral bone, trochanters, etc.) against with bed. Timely and correctly performed NVP reduces the risk of neurotrophic complications (decubitus) silent aspiration, pathologic (pain) sensitization, joint damage, and stricture formation. It contributes to the optimal lung ventilation and sputum clearance, provides a comfortable medium for a patient and adequate perception of the surrounding space, and optimizes the conditions for hygienic care manipulations. Unlike VP, NVP is not associated with an increase in a patient’s energy demands. Thus, it can be applied in the acute period of the critical condition.
Mobilization is a strategy of patient activity management in the conditions of artificial immobilization and bed-rest. It involves active and passive movements in all joints and verticalization. Early mobilization is an increase in physical activity of an ICU patient in the period of 2 to 5 days from admission.
Kinesiotherapy (KST) (Greek “kinesis” — movement + therapy) is the primary method of therapeutic exercises used by MDRT specialists during the mobilization of ICU patients. It includes active and passive approaches depending on the level of consciousness and movement deficit.
Stretching. Passive stretching is a manipulation that involves light stretching of ligaments and muscles during joint gymnastics in ICU patients. It works as a short-term (up to 10 seconds) fixation of muscle and ligament apparatus in a slightly stretched condition in the limiting range of the anatomical movement of the joint. Stretching is performed by a specialist in kinesiology as an element of passive joint gymnastics. During the stretching, the generation of potential occurs as the primary element of the motor proprioception, which imitates the effect of the active muscular contraction, contributes to an increase in a patient’s wakefulness, and prevents the learned non-use effect.
Joint Gymnastics is a basic method of early mobilization aimed to prevent hypokinesia as a trigger for the formation of contractures during immobilization. Joint gymnastics can be performed by a patient themselves (active) or with the help of a specialist in physical and rehabilitation medicine (passive). The general principle of joint gymnastics is in active (passive) continuous movements in the main joints of the upper and lower limbs.
Handling is a series of manipulation with the body position of a child to optimize its positioning. It is a therapeutic and preventive manipulation. The patient’s parent (caregiver) provides the optimal position on their hands with optimal exposition to prevent complications during immobilization in children from 0 to 3 years old.
Ergotherapy (Lat. ergon — labor, occupation, Greek therapia — therapy) is a complex of measures that aim to restore self-care skills and independence in patient’s routine life to the premorbid level.
Acute period of critical illness, which requires ICU therapy, corresponds to the lowest level of personal independence of a patient in the evolutionary process of sanogenesis. This occurs because of partial or complete loss of self-sufficiency induced by ICU technologies of apparatus monitoring that partially or completely substitute the patient’s vital functions. With successful outcome of the intensive therapy, the patient will need to restore self-sufficiency in everyday life, which can either return to the premorbid level or decrease depending on the individual reparative processes. The paradox of intensive care is in the fact that a complex of life-saving technologies can lead to a long-term and incomplete restoration of the quality of life. The effect can be more significant than after the emergency condition itself that required intensive care. This condition is called Post Intensive Care Syndrome (PICS). This term first appeared at the beginning of the 21st century in the materials of the conference on multidisciplinary cooperation of reanimatologists and specialists in rehabilitation [1, 2]. The Russian term for PICS is “Syndrome Posledstviy Intensivnoy Terapii” or “PITS” [3].
Staying at the ICU or specialized units for intensive care at the Traumatology, Cardiology, and Surgery Departments is the 1st stage of treatment in a medical center for patients with critical illness or at the early post-operative period after planned surgery or other therapeutic-diagnostic manipulations that require all-day monitoring. The need for medical rehabilitation at the 1st stage of intensive care is determined by the requirement in the prevention of PICS, which is directly associated with ICU period [1, 7–9].
The data on the key symptom complexes, risk factors for their development, and evolution in the post-reanimation period are presented in Table 1. The data are collected from various publications on PICS [9–15]. PICS includes only those syndromes that do not have direct cause-effect relations with patient’s critical condition that resulted in the ICU hospitalization.
Table 1. Structure and Risk Factors for PICS (edited by A.A. Belkin)
| No. | PICS symptom complexes | Risk factors | PICS manifestation in ICU | PICS complications |
|---|---|---|---|---|
| 1. | Infectious and Trophic Complications | |||
| Nutrient deficiency Inadequate positioning | Decubitus | Chronic trophic ulcers | ||
| Tracheotomy Long-term nasotracheal and orotracheal intubation |
Respiratory tract infections | Tracheoesophageal fistula Sinusitis Post intubation tracheal stenosis |
||
| Long-term bladder catheterization | Urinary tract infection | Urethral stricture Epicystostomy |
||
| Immobilization/bed-rest | Lower limb thrombosis and embolism | Secondary trophic lesions and risk of thromboembolism | ||
| 2. | Vegetative and Metabolic Complications | |||
| Chronic pain syndrome | Inadequate analgesia Underdiagnosis of pain triggers and pain behavior |
Persistent sympathetic hyperactivity (hypertension, tachycardia, hidrosis, paroxysmal attacks, etc.) | Chronic pain syndrome (visceral, musculo-skeletal, arthral, neuropathic) that regresses within 6 months after adequate specific therapy | |
| Circadian dysregulation | Analgosedation ICU technological noise Night nutrition Constant light Premorbid: Administration of hypnotics Children: Sleep/wakefulness regime disturbance in infants and younger children |
ICU-acquired dyssomnia Constipation Urine retention Children: Increased irritability, tearfulness, negative attitude to medical personnel |
Chronic dyssomnia that regresses within 1 year Long-term pelvic organ function disorders |
|
| Gravitational gravity disturbance | Immobilization/bed-rest Positioning with a bed head inclined down |
Orthostatic insufficiency | Disorders in static co-ordination, impaired walking coordination that regresses proportional to the duration of bed-rest up to 6 months | |
| Physical load tolerance reduction | Premorbid status of low activity Reduction of respiratory volume and decrease in pulmonary vital capacity Decrease in systolic output Senior age Immobilization/bed-rest Nutritional deficiency |
Reduced stamina Oxygen dependency |
Decrease in the routine activity because of a persistent decrease in tolerance to physical loads Prognosis: improvement within a month with residual activity deficit within 1 year in 50 % of patients |
|
| 3. | Neuromuscular Complications | |||
| ICU-acquired weakness (ICU-AW) | Immobilization/bed-rest Body weight loss Nutritional deficiency Myorelaxant Corticosteroids Sepsis Multiple organ failure |
Decrease in muscle strength, primarily in hands Peripheral tetraparesis |
Persisting loss of muscular mass in 55–95 % of patients aged 2–5 years old Fine motor skills impairment |
|
| Decrease in the volume of active movements in large limb joints | Soft tissue contractures in the distal joints (ankle, radio-carpal) | |||
| Spasticity in distal regions | ||||
| Heterotopic ossification | ||||
| Respiratory ICU-acquired weakness [5] | Continuous Mandatory Ventilation (CMV) with controlled mods Immobilization/bed-rest Pneumonia |
Decrease in lung vital capacity and respiratory dependence on CMV Weakening of cough reflex Hypophonia |
Decreased tolerance to loads, elongation of withdrawal from CMV | |
| ICU-acquired dysphagia (learned non-use) | Tracheoesophageal separation (tracheostomy, endotracheal tube) for over 72 hours Nutritional learned non-use Premorbid: Cerebral strokes in medical history |
Silent aspiration after decannulation Impossibility of per oral nutrition |
Recurrent aspiration pneumonia Cannulation Gastrostomy Body weight deficit, cachexy |
|
| Spontaneous recovery is possible within 2–4 weeks | ||||
| 4. | Emotional and Cognitive Complications | |||
| Cognitive impairments | Premorbid psychic disorders and low intellectual level Sedation < –2 RASS score Analgosedation Immobilization/bed-rest ICU-acquired cognitive-sensory dissonance Long-term CMV Nutritional deficit Hypoglycemia ICU-acquired delirium ICU-acquired dyssomnia Recollections on the time spent in ICU Female sex Premorbid: Application of antidepressants and/or neuroleptics Alcohol abuse Children: Primary behavioral pattern impairment Inadequate communication with the child Negative attitude to medical personnel Long-term immobilization |
Cognitive-sensory dissonance: space, time, and personality disorientation | Memory and attention disorders, 30–80 % of patients have cognitive impairments that can persist for 1–6 years with incomplete regression to the premorbid status | |
| Retrograde amnesia | Executive functions impairments | |||
| Poor agility | Neurodynamics reduction | |||
| Loss of self-care skills | Executive functions decline to complete apraxia | |||
| Emotional Impairments | Agitation | in 10–50 % of patients and 33 % of family members: symptoms of depression and anxiety, sleeping disorders can persist for over 4 years | ||
| Anxiety | Depression | |||
| Psychic Impairments | ICU-acquired delirium | Subacute mental impairments Increased risk of early dementia |
||
| 5. | Decrease in the Quality of Life in Comparison with Premorbid Status | |||
| Incapability to return to a premorbid way of life without rehabilitation | Social status decline (reduction of qualification, loss of job) Limited independence in everyday life (disability) |
|||
The terms PICS and chronic critical illness should not be confused. They have different pathophysiological basis, course of sanogenesis, and prognosis. PICS is known to predispose the development of chronic critical illness [16].
Despite a clear cause-effect relation between PICS and ICU therapy, PICS cannot be considered an iatrogenic complication from a physiological or legal point of view [17].
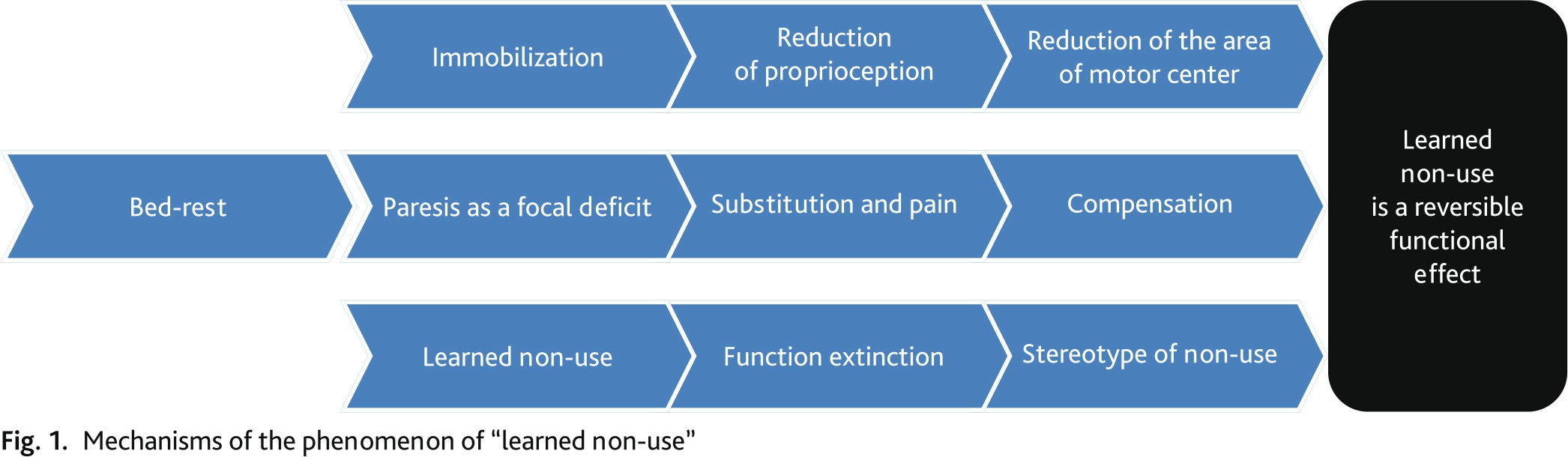
Pathophysiologically, immobilization syndrome (IS) is based on the so-called learned non-use or artificial functional inactivity. In short, functional inactivity and cognitive isolation contribute to sensorimotor separation, i.e. disorders in the integrity of conditional and unconditional reflexes [4]. The mechanisms of learned non-use are presented in Figure 1.
Fig. 1. Mechanisms of the phenomenon of “learned non-use”
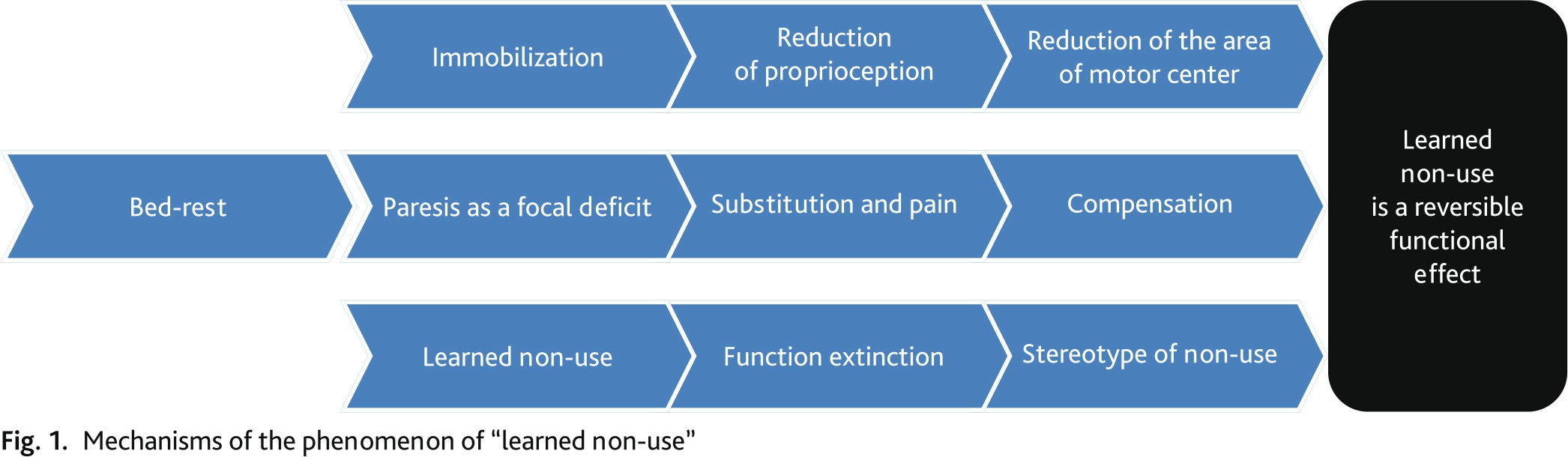
Therapeutic immobilization (TI) contributes to the development of learned non-use phenomenon. There are two types of TI. The primary TI is a result of activity limitations because of acute cerebral insufficiency (cerebral stroke, craniocerebral injury, spinal cord injury; CNS infections and intoxications, etc.) and neuromuscular diseases (polyradiculoneuropathy, myopathy, myasthenic crisis). The secondary or therapeutic immobilization is a combination of medical manipulations (bed-rest, sedation, myorelaxation, CMV, etc.) [16].
Classic model of TI is bed-rest. It is a method of a patient’s positioning in the ICU proposed by an English surgeon John Hilton in the XIX century (On Rest and Pain: a Course of Lectures on the Influence of Mechanical and Physiological Rest in the Treatment of Accidents and Surgical Diseases, and the Diagnostic Value of Pain, 1863) as the main therapeutic strategy of treatment for heavy patients. In the XX century, this practice turned into immobilization, which is an immobilized horizontal position of a patient maintained by sedation and myoplegia that provides metabolic rest during critical impairment of perfusion and oxygenation. TI contributes to the management of the most serious problems in the intensive care:
Along with this, immobilization demonstrated various multiple organs negative events that underlie PICS. Pathological manifestations of TI are described in Table 2 [3, 8, 9, 12, 13, 19].
Table 2. The main side effects and complications of therapeutic immobilization
| Musculoskeletal system | Decreased myoprotein synthesis |
| Muscular atrophy and a decrease in the general body weight | |
| Decrease in muscular force | |
| Decrease in the tolerance to physical load | |
| Shortening of tendons and contracture of joints with initial manifestations in 8 hours | |
| Bone resorption and hypercalcemia 1 % per week | |
| Joint tenderness | |
| Respiratory system | Decrease in the inspiratory pressure and vital lung capacity |
| Atelectasis | |
| Pneumonitis | |
| Cardiovascular system | Decrease in the overall size of the heart and left ventricle |
| Decrease in the venous compliance of lower extremity veins | |
| Decrease in the cardiac output (CO), systolic output (SO), and total peripheral vascular resistance (TPVR) | |
| Microcirculatory insufficiency | |
| Decrease in the cardiovascular reactivity to the stimulation of carotid sinus | |
| Metabolism | Neurotrophic disorders |
| Insulin intolerance | |
| Decrease in the activity of aldosterone and plasma renin | |
| Increase in the levels of atrial natriuretic factor | |
| Urogenital system | Urine retention |
| Increased risk of infection | |
| Urolithiasis | |
| Gastrointestinal system | Dysperistalsis |
| Constipation | |
| Nervous system | Orthostatic insufficiency |
| Cognitive isolation | |
| Post-traumatic stress |
Early and the most clinically significant complications after TI include ICU-acquired weakness, ICU-acquired dysphagia, a decrease in GG, cognitive-sensory dissonance, and ICU-acquired dyssomnia.
ICU-acquired weakness (ICU-AW) is a combination of myopathy and polyneuropathy, which is manifested as general muscular weakness. It is the main cause of difficulties in withdrawing a patient from CMV. Unlike other conditions that can lead to clinical manifestations of neuromuscular weakness in ICU patients, ICU-AW is an exceptional manifestation of PICS as an example of functionally complete or partial inactivity. An example of such a mechanism is respiratory ICU-weakness in patients on long-term CMV (over 7 days), which leads to difficulties in transfer to spontaneous breathing in 25 % of patients. The pathogenetic basis of this condition is a lesion of the neuromuscular apparatus of the external breathing, primarily the diaphragm, which thickness reduces by 25 % by day 7 on CMV [21].
Multi-organic insufficiency, fluid and electrolyte disorders, nutritional deficit, and the application of myorelaxant agents and glucocorticosteroids contribute to the progressing of PICS [22, 23].
ICU-acquired dysphagia (learned non-use) is a clinical symptom of swallowing function impairment, which prevents adequate enteral feeding and decannulation because of the risk of aspiration complications. ICU patients face neurogenic oropharyngeal dysphagia. Apart from the described above mechanism of “learned non-use”, long-term tube feeding, which excludes physiological three-phase swallowing leads to a) post-extubation dysphagia as a complication after long-term intubation that interferes with a physiological rate of swallowing movements (from 8 per hours during sleeping to 5 times per minute during eating); b) dysphagia caused by the lack of subglottic pressure during cannulation; c) dysphagia as a syndrome of ICU-acquired weakness [24, 25]. The application of analgosedation, which includes morphine and diazepam, contributes to the development of dysphagia [25].
Decrease in GG (Orthostatic Insufficiency). A redistribution of the blood in the vascular system when the body position changes from a horizontal to vertical one maintains stable vital parameters in any body position in relation to the gravitational field of the earth. The redistribution of blood occurs relative to some hydrostatically indifferent point, which is located several centimeters below the diaphragm level. This process is initiated by pulsation going from the labyrinth semicircular ducts and pressoreceptors in feet. In response to afferent stimulation, a complex reflex stereotype is executed. It targets an increase in the tonus of capacitance vessels below the diaphragm, a closure of some functional tissue arteriovenous anastomoses, primary increase in the tonus of peripheral arteries, and primary decrease in the tonus of cerebral arteries. As a result, the centralization of circulation occurs. It is characterized by the state when 300–800 ml of the blood, that are deposited in the relaxed vessels, are redistributed to elevate the preload and cardiac output. Increased mean blood pressure (mBP) in combination with decreased resistance of cerebral vessels provide normal cerebral perfusion pressure and prevents orthostatic reactions.
When the primary mechanism turns to be ineffective, a non-specific reflex occurs in response to hypotension:
When the specified mechanisms cannot maintain gravitational gradient, orthostatic insufficiency (OTI) develops, which is manifested as dizziness, visual impairment, cognitive deficit, loss of consciousness, falls, and dysautonomia (tachycardia, hyperhidrosis, pale skin, dyspnea, shoulder and neck algospasm, oliguria). In an ICU patient, the risk of OTI is increased by:
ICU-acquired dyssomnia. Among other vegetative disorders, issues with circadian rhythms occupy a certain place in the structure of PICS. Circadianity is a natural process that determines behavioral reactions in response to the changes in illumination. They include cyclicity of hormone production and sequence of sleep and wake. ICU conditions inevitably lead to their changes. Such factors as constant illumination, all-day manipulations, noise, night feeding, and other situations, that are normal for ICU but not physiologically natural, contribute to the development of these changes. Among the ICU “noises”, talks among medical personnel can have a significant negative effect on patient’s condition. Most other noises do not lead to patient’s awakening but still reduce the depth of sleep and cause its fragmentation. The developed dyssomnia (sleep impairment) persists for a long time after the patient’s discharge from hospital. It contributes to a decrease in the tolerance to physiological and mental loads as well aggravates the course of cognitive-sensory dissonance, which is another specific iatrogenic condition that determines PICS.
Cognitive-sensory dissonance is a condition characterized by an artificially reduced perception (sensory organs) and proprioception (internal organs). Perception impairment, in combination with disturbances of circadianity caused by long-term hypnotic drug-induced condition, provokes cognitive-sensory dissonance in ICU patients. Because of the lack of familiar sensations (odors, touches, relative’s voices), that are replaced by other negative and aggressive stimuli (monitors noises, moaning and inadequate speech of patients, rough replies of medical personnel, etc.), the patient faces impairments in the associative sphere and develops a condition of derealization and depersonalization. The most severe manifestation of cognitive-sensory dissonance is ICU-acquired delirium.
Physical complications after critical illness can develop in 70 % of patients [9, 54]. The total rate of PICS is around 20 % one year after ICU treatment [4, 15, 23]. Over 50 % of all ICU patients with novel coronavirus infection COVID-19 and 80 % of patients after CMV [10, 25], demonstrate the development of PICS [11].
The rate of immobilization-induced complications in patients with acute cerebral insufficiency (ACI) reaches 65–80 %, and in general ICU patients that spend > 48 hours in ICU, it reaches 55–60 % [14]. The rate of ICU-acquired weakness in adult ICU patients who spent > 2 weeks on CMV with sepsis or multiple organ failure is 46 % [15]. Around 50 % of patients with ARDS aged 45 years old cannot work within a year, and 33 % of patients have persistent disability. The first year mortality ranges from 26 to 63 %. Around 50 % of patients need assistance within the first year after the discharge [13].
Around 60 % of intubated patients show the signs of dysphagia, and around 50 % of intubated patients have aspiration. In 1/3 of orally intubated patients with acute respiratory distress-syndrome (ARDS), dysphagia persists after discharge. In 23 % of such patients, it remains within 6 months after discharge. Over 60 % of patients with acute respiratory failure (ARF) have swallowing impairments after CMV [33]. To compare, only 30 % of patients with cerebral stroke have primary neurogenic dysphagia [28].
Cognitive deficit is observed in 30–80 % of patients. It persists up to a year and may not completely regress to the premorbid level [15]. Not less than 10–50 % of patients experience symptoms of depression, anxiety, and long-term persisting sleep impairment [29].
PICS does not have its code in the ICD-10. The following codes can be used to describe its manifestations:
Some specialists believe PICS should be included in the International Classification of Diseases (ICD). Currently, specialists are actively searching for adequate combinations of codes, which opens perspectives in the personalized evaluation of the dynamics of patient’s condition during step-by-step rehabilitation [16].
Despite an increasing number of high-quality publications, there is still no international clinical classification of PICS (except single publications) [30]. The most acceptable variant for practical application is proposed by specialists of the Union of Rehabilitologists of Russia together with the Federation of Anesthesiologists and Reanimatologists of Russia. This approach on the evaluation of PICS using clinimetric scales allows the specialists to identify the main modalities of the symptoms and estimate their evolution during the treatment (see further).
Clinical picture of PICS is determined by the expression of its separate components detailized by the members of MDRT. For a resuscitator, a general picture is acute that motivates to expand the rehabilitation process and decide on further rehabilitation routing of a patient. A typical picture of ICU-acquired weakness can be observed in a patient in week 3–4 after the extended CMV. The volume of muscular mass and muscular force decrease, a patient cannot lift arms and legs or can hardly do that. The observed paresis is symmetrical and can prevail in both proximal and distal segments of the limbs. Pathological upward bending of the ankle (equinus) is registered. Rarely, paresis is observed in the oculomotor, mimic, and bulbar muscles. Muscular tonus and tendon reflexes are symmetrically reduced or absent. In the distal segments of limbs, a reduction in pain, thermal, and vibration sensitivity is observed. The skin of patients is dry and peeling. They have dermal derivatives with signs of trophic impairments. The above-mentioned symptoms indicate a combination of two syndromes: symmetric peripheral tetraparesis and neuro-muscular respiratory failure. After a withdrawal from CMV, spontaneous breathing is characterized by dyspnea with minor breathing volume, and the patient is anxious. During the lavage of the tracheobronchial tree, a reduced cough impulse is observed as a manifestation of decreased strength of respiratory musculature. For this reason, in combination with phase 1–2 swallowing impairment, transfer to per os feeding and decannulation is postponed. Patients experience disorientation in the current condition, place, and time. Often, they develop retrograde amnesia. The patient is reluctant to communicate or has difficulties with communication. The reaction to communication is slow and barely emotional. Patients have poor sleep quality and reduced appetite. Attempts of verticalization lead to the development of orthostatic insufficiency.
Clinically, PICS is like chronic critical illness (CCI) [16] but these two conditions are essentially different. CCI is a long-term multiple organ failure accompanied by the prevailing vital functions failure. PICS is a complex of symptoms that develop after acute condition relief, which complicates the recovery of the patient to the premorbid status.
Recommendation 1. It is recommended to evaluate the signs of PICS every 24 hours in patients of any age that spent over 48 hours in the ICU by all members of MDRT based on the clinical examination score (Annexes 2–14) [37–40] (level of evidence — 4, grade of recommendation — С).
Comments. The interpretation of results during diagnostic of PICS should include symptoms that are not associated with the primary disease. For example, signs of ICU-acquired weakness, dysphagia, depression, cognitive impairments, and dyssomnia in patients that had critical condition non-associated with central nervous system lesion are interpreted as manifestations of PICS. The criteria of PICS diagnostic are outlined in the National Guidelines on Intensive Care [41–43]. The analysis of the application of various clinimetric scales for the diagnostic and evaluation of PICS dynamic by MDRT specialist in 26 British intensive care hospitals during the pandemic confirmed their non-specificity (in the critical condition assessment) and sensitivity (in the dynamics assessment) during short-term ICU stay [30]. This provides the basis for upscale methodological approaches to PICS described in the National Guidelines, although they have not been fully validated yet [42]. Table 3 shows a complete list of clinimetric scales, normal values, and specialties of MDRT specialists responsible for the control and interpretation of the data according to the respective scale. The general rule of PICS diagnostic: the deviation from the normal clinimetric score should not be associated with the primary disease that led to the ICU hospitalization.
Table 3. A set of wedge and metric scales and distribution under the competencies of MDRT specialists
| No. | Modality of symptoms | Type | Clinical measurement[1] | Normal value | Designated MDRT specialist |
|---|---|---|---|---|---|
| 1 | Infectious and Trophic complications | Decubitus | Clinical and laboratory data, specific scales and metrics | Lack of clinical and laboratory manifestations | |
| Respiratory infections | Anesthesiologist- reanimatologist (AR, doctor) | ||||
| Urological infection | |||||
| 2 | Vegetative and Metabolic Complications | Pain | BPS (Annex 2) NIPS (children > 3 years old) (Annex 3) FLACC (children ≥ 3 years old) Eland body tool (children 3–7 years old) |
0/0 | AR (doctor) Physical medicine and rehabilitation physician (PRM physician, doctor) |
| Circadian rhythm impairment: dyssomnia | Sleep Quality Inventory (including children ≥ 7 years old) | 0 | PRM physician (doctor) | ||
| Decrease in gravitational gradient | Verticalization test in bed (semi-orthostatic test, sitting in the bed with legs down on the floor) (including children ≥ 7 years old) | PRM physician (doctor) Specialist in PM&R |
|||
| Decrease in the load tolerance | Borg scale (including children ≥ 14 years old) | < 4 | PRM physician (doctor) | ||
| Metabolometry | AR (doctor) | ||||
| Nutritional insufficiency | NRS scale (nutritional risk) | PRM physician (doctor) AR (doctor) |
|||
| Body mass index deficit | Body Mass Index (BMI) | > 18 | AR (doctor) | ||
| 3 | Neuromuscular complications | ICU-acquired weakness (ICU-AW) | MRC scale (Annex 4) (including children ≥ 14 years old) | > 3 in all the limbs | PRM physician (doctor) |
| Dynamometry (including children ≥ 14 years old) | Male > 10 kg Female > 6 kg |
Specialist in PM&R | |||
| Respiratory ICU-acquired weakness | Tobin Index (Annex 5) | >100 | AR (doctor) | ||
| ICU-acquired dysphagia (learned non-use) | Dysphagia outcome and severity scale (DOSS) | 0 | Speech and Language Therapist (SPL) |
||
| 3-ounce water swallow test [Annex 6] | Positive | MR Nurse ICU Nurse |
|||
| 4 | Emotional and Cognitive Complications | Memory and self-orientation impairments | A set of special tests (FAB, MMSE, MOCA) | Clinical Psychologist | |
| Delirium/Hallucinations | RASS scale | 0–1 | AR (doctor) | ||
| Anxiety/Depression | HADS (including children ≥ 14 years old) | 0 | Clinical Psychologist | ||
| Express test of PICS in patients | |||||
| Mobility | Rivermead Mobility Index (Annex 7) (including children ≥ 14 years old) [143] | > 6 | AR (doctor) | ||
| Communication | Hodkinson scale (Annex 8) [142] | > 7 | |||
[1] The text of the present methodical recommendations (Annexes 2–14) include only those clinical measurements that are used by MDRT specialists together with an anesthesiologist-reanimatologist. The rest scales and methods mentioned in the Table are described in the respective specialized guidelines.
Recommendation 2. It is recommended to apply non-validated index of PICS severity by the members of MDRT for the diagnostic and dynamic assessment of PICS in adult ICU patients (Annex 9) [44] (level of evidence — 5, grade of recommendation — С).
Comments. The calculation of PICS index is performed based on the sum of symptom ranging revealed by the members of MDRT. The score 0-10 shows the development of PICS, severity, and effectiveness of rehabilitation manipulations.
Recommendation 3. It is recommended to assess the condition of adult patients and PICS severity using express PICS-index (Annex 10) before transferring adult patients from ICU (level of evidence — 5, grade of recommendation — С).
Comments. PICS express test is a minimal set of clinimetric scales sufficient for PICS screening by AR if there is no licensed department of early rehabilitation (or other organization for MDRT specialists’ service) in a hospital. Express assessment is performed during the primary examination of a patient considering the data on the premorbid status and a transfer of this patient from ICU. The score is positive if a patient does not meet at least one normal value of mobility or/and communication, and this is not associated with the primary critical illness.
Recommendation 4. It is recommended to use the following criteria for PICS diagnostic in ICU patients of all ages:
Comments. ICU-acquired weakness is the most common and severe manifestation of PICS, which was shown by COVID-19 experience [19]. Thus, its diagnostics should be clear and reproducible not only for MDRT but also for AR [42].
Recommendation 5. It is recommended to use rapid shallow breathing index (Tobin Index) for the diagnostic of respiratory ICU-acquired weakness in adult patients on CMV [27, 32] (level of evidence — 3, grade of recommendation — B).
Comments. Tobin Index (Annex 5) is a rapid shallow breathing index (RSBI). This index demonstrated effectiveness in the evaluation of respiratory muscle failure in patients after CMV during a transfer to spontaneous breathing [1]. Tobin Index has several advantages: high sensitivity (0.97) and specificity (0.64), it is easy to evaluate; it does not depend on the effort and cooperation of the patient, and has a high prognostic value [27, 28]. The establishment of high RSBI in a patient with other normal parameters of pulmonary mechanics is a sign of respiratory muscle weakness, i.e. respiratory ICU-acquired weakness [33].
To prevent PICS, specialists of the Union of Rehabilitologists of Russia together with the Federation of Anesthesiologists and Reanimatologists of Russia proposed a rehabilitation complex “RehabICU” [41, 42]. RehabICU aims to preserve premorbid status of patients’ socialization by preventing the PICS syndrome, which develops because of immobilization, cognitive, and socially routine limitations. These limitations are inevitably associated effects patients face during intensive care that are essential for the treatment and resolution of the critical state. In the English-language publications, this complex is called “Awakening and Breathing Coordination, Delirium monitoring/management, and Early exercise/mobility” (ABCDEF) bundle [37].
The first upscale experience of the application of rehabilitation technologies in ICU was obtained during COVID-19 pandemic, when major ICU centers had teams of early rehabilitation organized. The results of RehabICU show a decrease in the requirement for further stages of rehabilitation and an increase in the quality of life of the survived patients [30, 40].
Recommendation 6. It is recommended for ICU patients of any age, that spend > 48 hours in the ICU, to receive prevention of PICS syndrome regardless of the disease nosological entity, type of surgical intervention, severity of the condition, and respiratory status [35, 38, 46] (level of evidence — 2, grade of recommendation — A).
Comments. The main syndromes that indicate PICS include [19, 21, 29, 50, 54]:
According to various multicenter studies [44, 46], a combination of PICS signs into technologic therapeutic and diagnostic modules “positioning and mobilization”, “prevention of dysphagia and nutritional deficiency”, “prevention of emotional and cognitive impairment and delirium”, “prevention of loss of self-care skills” can provide diagnostic screening and a complete spectrum of rehabilitation care to ICU patients. The algorithm of cooperation between AR and MDRT is described in Annex 1.
Recommendation 7. It is recommended to perform a daily individual program of rehabilitation for all ICU patients. The program should last not less than 1 hour and not more than 3 hours considering the status of consciousness and the level of mobility, and paying special attention to the respiratory status of a patient to prevent PICS [35, 36, 39, 40] (level of evidence — 3, grade of recommendation — B).
Comments. Depending on the possibility of patient’s participation in the rehabilitation measures (severity of the condition, level of consciousness), the rehabilitation should be performed in an active, passive, and active-passive regimens. The program of rehabilitation [35] should include a combination of methods of kinesiologic manipulations (positioning, verticalization, mobility, velokinetic loads, and electroneuromyostimulation) as well as practices of clinical psychologists, ergotherapists, and medical SPL [37]. The specific weight of kinesiometric chronometry (KST) should be not over 50 % [39]. The nomenclature of the main and adjuvant kinesiotherapeutic practices is presented in Annex 11.
Recommendation 8. Daily rehabilitation is not recommended for patients who spent less than 48 hours in ICU, including those who underwent intubation, CMV, and uncomplicated cardio surgical intervention [46] (level of evidence — 3, grade of recommendation — B).
Recommendation 9. It is not recommended to start rehabilitation manipulations on mobilization and verticalization if a patient has absolute contraindications. The contraindications should be evaluated daily regardless of the presence the day before (Annex 12) [47–49] (level of evidence — 3, grade of recommendation — A).
Recommendation 10. It is not recommended for ICU patients of all ages to perform rehabilitation measures on mobilization and verticalization without proper hemodynamic monitoring because of the risk of RehabICU complications [47–49] (level of evidence — 3, grade of recommendation — A).
Recommendation 11. It is recommended to stop rehabilitation procedures on mobilization and verticalization in ICU patients of all ages when their monitored parameters deviate from the norm and STOP-signs develop (Annex 12). It will prevent RehabICU complications [47–49] (level of evidence — 3, grade of recommendation — B).
Comments. STOP-signs include signs that show the maximal rate of reproducibility obtained during a thorough analysis of publications and clinical experience of ICU departments that use clinical recommendations of the Union of Rehabilitologists of Russia together with the Federation of Anesthesiologists and Reanimatologists of Russia during the novel coronavirus infection (COVID-19) pandemic [43, 44]. The presence of STOP-signs is evaluated by non-validated specialized BPS scales (Annex 4). If any of these symptoms appear, RehabICU should not be started or should be stopped. If STOP-signs develop during verticalization, the procedure should be stopped and the patient should be returned to the initial position (lower by 200) or lower to 0° without stopping at the angle of elevation [65]. In children, sedation is an obstacle to early mobilization. Sedation in children differs from sedation in adults because of safety issues and evaluation of pain and anxiety in small children [67]. The level of evidence of the signs specified in the Table is not higher than C. But it is difficult to obtain qualitative evidence for patients in ICU because of ethical issues of the formation of the control group in such studies.
Recommendation 12. It is recommended to perform passive leg raising test (Annex 13) in adult ICU patients before the beginning of each session of manipulations on mobilization and verticalization for the evaluation of the risk hemodynamic STOP-signs during these procedures [56, 57] (level of evidence — 3, grade of recommendation — B).
Comments. On the one hand, positive passive leg raising test shows hypovolemia, which will lead to orthostatic insufficiency during verticalization, which is unfavorable in patients in critical condition. On the other hand, this situation should not be considered an absolute contraindication for mobilization. The causes and the plan of euvolemia restoration should be evaluated. If the results are negative during the repeated testing, the realization of the rehabilitation plan should be resumed [56].
Recommendation 13. It is recommended to perform non-vertical positioning (handling for children) for ICU patients of all ages within the 1st day in the ICU. It should be made by changing the position of limbs and body of the patient in relation to the horizontal plane depending on the status of verticalization not rarer than every two hours (except for night sleep) to prevent complications after therapeutic immobilization [59, 62] (level of evidence — 3, grade of recommendation — B).
Comments. Unlike mobilization, non-verticalizing positioning does not have absolute contraindications. It should be applied starting from day 1 regardless of the volume of other modalities of early rehabilitation by the medical personnel in charge [65]. Positioning is used for gravitational stimulation during the head bed end elevation. Thus, the head bed end should always be elevated > 300. Consecutive changes of the body position of the patient are made on a three-section bed with the formation of the position according to the status of verticalization. The manipulation aims to enable the patient to spend more time in the semi-sitting or sitting position (elevated head bed end and lowered feet bed end). The specialists help patients to change poses when lying on the bed (on the right and/or left side, or on the back), on an elevated head bed end, or in a sitting position. It should be noted that bending should be made in the pelvic joints and not in the thoracic and lumbar sections. To avoid reflex impairments of the muscular tonus, the supine body position should always be symmetrical. Body position on the side contributes to better drainage function and prevents sputum retention [64]. Positioning on an elevated head bed end and in a sitting position with complete support increases the breathing capacity and contributes to effective expectoration [65]. In all cases, free feet drop should be avoided using any support for irritation of the feet receptors. It should be remembered that none of these variants of positioning is ideal. Any of these positioning variants have their indications and contraindications. The specialists should choose the optimal poses and their sequence individually. This will prevent complications and provide safe early mobilization and verticalization of a patient. It is necessary to consider individual tolerability and STOP-signs (Annex 12).
Recommendation 14. It is recommended to start active-passive mobilization, including verticalization and vertical positioning, in all ICU patients of all ages not earlier than 24 hours and not later than 72 hours after the onset of critical Illness (postoperative period) or directly after deciding on the lack of contraindications to the beginning or continuation of mobilization (Annex 3) to prevent complications after immobilization [73, 140] (level of evidence — 2, grade of recommendation — B).
Comments. Early mobilization is an element of rehabilitation process for patients in the ICU [35, 42]. Early mobilization is a process of improvement of a patient’s functional activity, in particular, a patient’s ability to turn in bed, sit, stand up, and walk as soon as possible. Minimal but self-maintained muscular activity prevents the development of muscular atrophy as an early sign of immobilization syndrome. Rehabilitative activities on mobilization of ICU patients are divided into two types regarding involvement of the patient. The first type is active; it is used for patients capable of cooperating with MDRT specialists. The second type is passive; it is used for patients with low quantitative and/or altered qualitative level of consciousness.
During the planning of daily activities, MDRT specialists evaluate the patient’s condition using mRMI-ICU scale (Rivermead mobility index) (Annex 7). The score shows patient’s mobility. Together with the level of consciousness, this score is used to create a model that is used as a basis for the development of the mobilization program [35–44].
Recommendation 15. It is recommended to use kinesiotherapeutic methods (active-passive movements in all joints with stretching, active-passive veloergometry, sitting up with support, keeping balance in a sitting position, walking to a chair, keeping balance in a standing position, walking in place) for the mobilization of all adult ICU patients [38, 58, 76] (level of evidence — 2, grade of recommendation — B).
Comments. Mobilization is one of the rehabilitative interventions, which facilitates the movements of patients and increases the consumption of energy to improve the outcomes. Mobilization optimizes respiration, central and peripheral perfusion, muscular metabolism, and reduces the risk of venous clotting in the lower limbs.
Passive mobilization for non-cooperative patients includes a series of 10 repetitions of passive movements (passive articular gymnastics) in each major joint (interphalangeal, radio-carpal, ulnar, shoulder, pelvic, knee, ankle, and intermetacarpal) with light stretching in the limiting points of a physiological volume of movements. There manipulations are performed by a PRM specialist not less than twice a day. Besides, passive kinesiotherapy can be performed using mechanical simulators (including robotized) that provide cyclic training for separate joints and have sensors for the evaluation of the patient’s contribution in the active-passive mode. Passive-active velokinesis with a bed-side veloergometer for lower/upper limbs with the function of reverse movement and dosed resistance can be used as a preparation for verticalization.
Active kinesiotherapy is a series of exercises with active involvement of the patient for the maintenance and an increase in the movement activity necessary for verticalization. Active mobilization aims to train the patient and control available self-produced movements of the patient in all joints (active articular gymnastics) that include 10 repetitions 3-6 times per day. The realization of this recommendation will be affected by the quality of the organization of rehabilitative/mobilization measures in the ICU [16].
Recommendation 16. Kinesiotherapeutic procedure < 30 minutes per day are not recommended for adult ICU patients because of their low effectiveness [55, 58] (level of evidence — 2, grade of recommendation — B).
Comments. Maximal effect (reduction of CMV time) was achieved in patients that received > 30 minutes of daily exercises, including cyclic veloergometry [55]. Exercises < 20 minutes in patients on CMV per session and less than twice a day are ineffective.
Recommendation 17. It is recommended to include exercises with individually chosen gradually increasing level of graded load for ICU patients of all ages (simple limb raising, limb raising with load, overcoming resistance of elastic belts for the prevention and loss of muscular mass and decrease in the load tolerance) [78] (level of evidence — 2, grade of recommendation — B).
Comments. A meta-analysis [78] showed that the inclusion of exercises for resistance overcoming contributes to the preservation of muscular mass in the conditions of the therapeutic immobilization of a critical patient, provided the protein consumption is > 1.3 g/kg/day. The prevention of PICS without muscular activity is less effective even if the protein-energy balance is adequate.
Recommendation 18. It is recommended to perform passive verticalization for ICU patients of all ages with low level of self-mobility based on the technical possibilities to prevent orthostatic insufficiency [40, 59, 60] (level of evidence — 2, grade of recommendation — B).
Comments. This section of mobilization takes a special place in the structure of RehabICU because it significantly reduces negative effects of bed-rest and prepares the patient for transfer from ICU to another department as soon as possible [61]. A detailed protocol of verticalization is presented in the respective clinical recommendations [60] [http://rehabrus.ru/index.php?id=55]. During the procedure, a continuous multimodal monitoring should be performed for early diagnostic of STOP-signs (Annex 5).
Recommendation 19. It is recommended to perform daily manipulations on the verticalization with further positioning for ICU patients of all ages. The manipulations should start with a head bed end elevation (30–60°) to a sitting position with patient’s feet lowered to the floor and standing nearby the bed for gradual restoration of GG [59, 61, 62] (level of evidence — 3, grade of recommendation — B).
Comments. Maximal point of the head bed end elevation (the upper part of the body) regarding the horizontal plane that does not provide orthostatic insufficiency is called patient’s GG [35]. In healthy people, it is 900 and corresponds to the standing position. Standing is the best position of the body for effective respiration and maintenance of lung capacity. Until a patient feels well, they need to increase gradually the time of standing. The higher is GG and the time of patient in it, the lower is the risk of aspiration, decubitus, ICU-acquired weakness, contractures, pathological (painful) sensitization, and other PICS factors.
Patients with spontaneous breathing and patients on CMV should aim to maintain maximally long vertical antigravitation positioning at the level of GG [59] achieved during passive verticalization. In cooperative patients, GG is evaluated by the individual request of a patient. Such patients should be trained to bend forward. This is a position that allows the gravity force to help drain excretion from the posterior-inferior segments of the lungs.
The manipulations on verticalization should last 30 minutes 3 times a day. The duration of the procedure depends on the tolerability. Still, it should be more than 15 minutes. For example, the elevation of the head bed end to 60° (lower edge of the pillow should be above the scapulae to avoid excessive tension of the head and neck, a pillow should be placed under the popliteal space to relax the abdomen and lower limbs). In any position, the head should be in the position along the midline to prevent obstacles in the venous outflow, secondary increase in the intracranial and intraocular pressure, as well as an increase in the pathological muscular tonus in the paretic limbs [65]. In younger children (0–6 years old), verticalization starts from 0-10° to the level of verticalization that is suitable for the patient’s age. It is performed on parents or caretaker’s hands with handling manipulations [68].
Recommendation 20. It is recommended to use the method of selective respiratory training of the main and additional inspiratory muscles for adult patients on CMV, including special static and dynamic respiratory exercises like manual or apparatus percussion therapy (VEST) for the prevention of respiratory ICU-acquired weakness [65] (level of evidence — 2, grade of recommendation — B).
Comments. Procedures that target a reduction of dyspnea, improvement of tracheobronchial clearance, training of the skeletal muscle, and maintenance of the level of self-care are indicated during the period of transfer to spontaneous breathing. Right after the transfer, an expiration with positive pressure can be used. It is feasible to use simulators of stimulating spirometry (like Akapella, Сoach), equipment with high frequency intra/cardiopulmonary fluctuations (for example, TheVest, MetaNeb, Percussionaire), and electrostimulators of the diaphragm and intercostal muscles [44, 65, 73]. It is effective to use speaking valve, which creates useful air resistance and contributes to the improvement of emotional status of the patient, to restore vocal breathing [106–108]. All these manipulations have limitations in patients with the novel coronavirus infection because of the risk of infection to the personnel [40].
Recommendation 21. It is recommended to perform respiratory exercises, in particular, CPAP-therapy and active exercises on diaphragm (deep) breathing, in adult patients after cardiosurgical interventions to prevent hypoventilation [69, 70] (level of evidence — 2, grade of recommendation — B).
Comments. According to some studies, routine respiratory exercises did not prove to be effective after uncomplicated coronary artery bypass grafting [71]. However, it was established that patients, that did exercises on deep breathing after surgery, had significantly smaller atelectatic areas and better pulmonary function on the fourth post-operative day in comparison with the control group where patients did not perform such exercises [72]. Oxygenation was significantly elevated in patients that performed 30 deep inspirations within the first two post-operative days in comparison with the control patients that made 10 deep inspirations per hour [73].
Recommendation 22. It is recommended to perform daily sessions of spontaneous breathing during the sedation withdrawal in combination with verticalization manipulations added with active exercises for upper limbs to prevent respiratory ICU-acquired weakness in adult patients on CMV [74–76] (level of evidence — 3, grade of recommendation — B).
Comments. Issues with CMV withdrawal are associated with the incapability of respiratory muscles to restore lung ventilation [64]. High effectiveness of respiratory muscles (ratio of load and muscular capacity (PI/PI max)) is the main cause of patients’ dependence on CMV and a predictor of successful withdrawal from CMV. This is contributed by insufficient lung ventilation, respiratory muscles weakness, respiratory muscles fatigue, enhanced breathing, or cardiac failure [62, 63]. Dysfunction of respiratory muscles in mechanically ventilated patients is observed in 80 % of ICU patients, which indicated a decrease in the transdiaphragmatic pressure by 2-4 % per day within the first week of the ICU [73]. This observation confirms the suggestion that well-balanced periodical load on respiratory muscles during mechanical ventilation can be useful to prevent atrophy. It was shown that such methods of induction of (interrupted) load on respiratory muscles as spontaneous breathing and early mobilization increase muscular strength. In patients that were withdrawn from CMV, adding exercises for upper limbs enhanced the influence of general mobilization on the parameters of fatigue resistance during physical load and dyspnea [77].
Recommendation 23. It is recommended to apply electrostimulation of muscles to prevent short-term and remote complications of PICS in adult patients with long-term hospitalization, including patients on CMV [79] (level of evidence — 2, grade of recommendation — B).
Comments. Electrical stimulation of muscles (EMS) was studied as a method of treatment to prevent ICU-acquired weakness. It includes the application of percutaneous electrodes on the skin. These electrodes activate the underlying nerves for the creation of isometric muscular contraction. The treatment includes minimal joint movements and does not require cooperation with the patient. EMS therapy applied during the study lasted 30–60 minutes daily for at least 4 days. Three systematic reviews, that included 8 randomized studies, showed that EMS can be an effective manipulation for critical patients and contribute to the maintenance of muscular mass in the ICU conditions, especially in patients on CMV with long-term ICU stay [79, 80]. The meta-analysis contained 6 randomized clinical studies that included 718 patients. There were no significant differences between EMS and regular therapy by the global muscular strength, lethality rate, and ICU time in comparison with standard rehabilitation of critically ill patients. On the contrary, the results of another meta-analysis [81], which included 11 randomized controlled studies and 576 patients, showed that early application of EMS in ICU patients reduced the time of CMV, ICU time, and general number of bed-days in the hospital. In the future, it can have a positive effect on the quality of patient’s life due to the improvement of a patient’s capacity to perform routine activities. However, there is no evidence that EMS can improve the functional status of ICU patients during hospitalization, contribute to early awakening after general anesthesia, or decrease lethality (р > 0.05).
Recommendation 24. It is recommended to perform medicinal modulation (inosine + nicotinamide + riboflavin + succinic acid) in adult ICU patients with signs of PICS to increase the effectiveness of mobilization [82] (level of evidence — 3, grade of recommendation — B).
Comments. The only study dedicated to the influence of medicinal effect on the effectiveness of PICS therapy showed that a combination of kinesiotherapeutic manipulations and infusion injection of Cytoflavin did not influence the rate of restoration of GG during verticalization. Still, metabolography results lead to an increase in the consumption of oxygen. The authors concluded that the application of drugs with components of energotropic effect can have a positive modulating effect on an increase in the tolerability of rehabilitation measures on the prevention of PICS in various categories of patients [82].
Recommendation 25. It is recommended to evaluate nutritional status of adult ICU patients using NRS 2002 scale as an obligatory element of planning of an individual program of early rehabilitation [89] (level of evidence — 1, grade of recommendation — A).
Comments. The evaluation of nutritional status is an obligatory element of the evaluation of ICU patient from the moment of hospitalization. Medical history data and results of clinical examination and laboratory parameters, combined in NRS 2002 scale (Nutrition Risk Screening) [90], provides a picture of nutritional deficit for further planning of nutritional support within the guidelines of the Union of Rehabilitologists of Russia [94].
Recommendation 26. It is recommended to use the results of indirect calorimetry, performed at rest and during rehabilitation measures, in all adult ICU patients, provided if there is a technical possibility for the formation of an individual program on nutritional support [89] (level of evidence — 3, grade of recommendation — B).
Comments. It is known that muscles contain the largest pool of protein in a human organism. Critical illness is associated with expressed proteolysis and loss of muscular mass (up to 1 kg/day), which is associated with ICU-acquired weakness [95]. This is described in the recommendations on preparing a nutritional program with a simple nomogram: energetic requirements = body mass x 20–25 kcal/kg/day. The protein requirement is 1.3 g/kg [89]. Such approach does not account for individual peculiarities of a patient as well as metabolic needs during the rehabilitative process, especially, mobilization manipulations. Enough publications showed that patients with low body mass index and insufficient protein-energetic provision have very low tolerance even to the procedures of passive mobilization [96]. Still, it was shown that active kinesiotherapy and bedside velocycling increase energy consumption, which should be accounted for during planning of the composition and schedule of nutritional support [97]. Considering these facts, the optimal method for the evaluation of the individual need in the caloric consumption is an indirect calorimetry using a metabolograph. The application of metabolography [89, 9] increases the safety of rehabilitation because critical changes in the levels of CO2 in the exhaled air develop earlier than hemodynamic STOP-signs [98].
Recommendation 27. It is recommended to provide nutritional support of 30–35 kcal/kg of body mass/day and protein 1.5 g/kg of body weight for all adult patients with a high risk of decubitus development [91, 92] (level of evidence — 3, grade of recommendation — B).
Comments. The maintenance of the sufficient level of protein after its loss and/or utilization as well as rational calculation of energetic needs of an organism and their correction, decreases the risk of decubitus development in adults and contributes to the acceleration of rehabilitation in patients that already have decubitus.
Recommendation 28. It is recommended to apply progressive increase in the daily content of protein and calories in the enteral mixtures to the calculated target values to prevent overfeeding in adult patients starting from the first day in the ICU [89, 93] (level of evidence — 3, grade of recommendation — B).
Comments. Gradual nutritional support is sufficient for the correction of macro and micronutrients and compensation of energy in ICU patients. The excessive feeding (compensation for energetic needs of an organism in the volume ≥ 110 % from the target one) can contribute to an increase in the levels of glucose in the blood plasma and lead to additional need in the administration of insulin to the patient. Excessive feeding is associated with an increase in the risk of infectious complications and lethality.
Recommendations 29. It is recommended to perform the screening of postextubation dysphagia (PED) with a 3-ounce water swallow test (Annex 6) right after extubation in adult ICU patients with temporary tracheoesophageal separation (endotracheal intubation in combination with a nasogastric tube) for > 48 hours for the evaluation of the risk of aspiration and planning of the schedule of nutritional support [100, 101] (level of evidence — 3, grade of recommendation — B).
Recommendation 30. It is recommended to provide special dense liquid with the jelly viscosity for drinking to adult ICU patients within the first 48 hours after tracheal decannulation to prevent aspirational complications [100, 104] (level of evidence — 5, grade of recommendation — C).
Comments. The rate of post-extubation dysphagia in ICU patients reaches 18.3 % before transfer from the ICU; out of them, up to 80 % of patients preserve the signs of dysphagia after the discharge from the hospital [105]. Silent aspiration is registered in 36 % of patients. With postextubation dysphagia, manipulations should be performed on the restoration of swallowing function under the control of a SLT specialist from MDRT [35, 107]. Sometimes, an individual choice of the food texture should be made using special tests [107, 109]. If it is impossible, dense liquids should be used, which reduce the aspirational risk [103].
Recommendation 31. It is recommended to perform daily swallowing activities as well as combined taste and thermal stimulation in all patients with tracheoesophageal separation (endotracheal intubation or tracheostoma) to restore normal swallowing and prevent post-extubation dysphagia [100, 105] (level of evidence — 4, grade of recommendation — C).
Comments. A logopedic complex of patient management with tracheoesophageal separation because of endotracheal intubation or tracheostoma, especially on CMV, has its peculiarities that are not still included in a special protocol. Logopedic practice in ICU patients showed that differential logopedic massage, passive and active articulation gymnastics, swallowing exercises, stimulation of oral mucous membrane sensitivity, maintenance of taste sensations, and oral cavity hygiene prevents the development of dysphagia and spread of bactericidal flora to the lower respiratory tract [24, 107]. In turn, the effective prevention of dysphagia minimized the risks of complications after nasogastric feeding (nasopharyngitis, sinusitis, stricture, decubitus) and facilitates the normalization of nutritional status [109].
Recommendation 32. It is recommended to perform multi-component non-pharmacologic intervention, that includes mobilization, optimization of analgosedation, normalization of sleep, maintenance of cognitive status and level of routine adaptation, in adult ICU patients to reduce the risk of delirium [35, 84, 88] (level of evidence — 3, grade of recommendation — B).
Comments. Currently, there is no data from evidence-based medicine on the methods of pharmacological [113] and combined prevention of ICU-acquired delirium. None of the studied strategies led to a decrease in the rate of delirium [112]. Still, it is believed that multi-component interventions from the MDRT team can minimize the risks of cognitive impairments and delirium [114–116].
The prevention of delirium and other emotional and cognitive impairments is based on the fulfillment of the main requirements of the guideline protocols on algosedation as the main priority in the prevention of PICS [86]. The valid guidelines of the Federation of Anesthesiologists and Reanimatologists of Russia [87] include a regular screening of the pain status of a patient regardless of the level of consciousness and its balanced pharmaceutical control.
Combined physical exercises and cognitive training positively affect the proliferation of neutrons, decrease in the tumor necrosis factor (TNF)- α, interleukin (IL)-1, -6, -8, and C-reactive protein [82]. In turn, these changes contribute to the normalization of the brain structure (increase in the frontal and temporal density of the gray matter) and neuronal activation. They also decrease the astrocytic and microglial activity [decrease in S — 100β and glial fibrillary acid protein (GFAP)], which is clinically manifested as a reduction of the risk of delirium and minimizes remote emotional-cognitive impairments [88].
Multi-component rehabilitation program of prevention contains simple complexes of limb movements, cycles of spontaneous breathing, maintenance of the relevant level of orientation in space and time (which is contributed by the application of an acoustic apparatus, glasses, watches, removable denture) [114, 115], measures to provide nocturnal sleep, and basic activities on self-care [35, 110].
Recommendation 33. It is recommended for parents or caregivers to be with children in the ICU, if they follow the rules and regulations of being in the ICU, for the prevention of emotional-cognitive impairments and delirium [117, 134] (level of evidence — 3, grade of recommendation — B).
Recommendation 34. It is recommended to evaluate daily the expression of the pain syndrome in all ICU patients, regardless of the level of consciousness. If there are signs of pain syndrome, treatment should be started for the prevention of cognitive-afferent dissonance [85, 121] (level of evidence — 3, grade of recommendation — B).
Comment. The pain at rest is affected by psychological (for example, anxiety, depression) and demographic factors (for example, young age, one or several comorbid diseases, surgeries in medical history).
During a procedure, the perception of pain is affected by the intensity of pain before the procedure, type of procedure, main surgical or posttraumatic diagnoses, and demographic factors (junior age, female sex). Pain self-assessment scale is a gold standard for the assessment of pain in patients that can communicate adequately. Among adult patients in a critical condition that can speak about the pain they feel, the score can vary from 0 to 10. The self-assessment can be made orally or visually. It is the most reproducible pain intensity scale in clinical practice. Behavioral Pain Scale (BPS) (Annex 2) is the most reliable tool for the monitoring of pain in the postoperative, general, and traumatologic ICU for barely cooperative patients with controlled behavioral reactions and movement functions that cannot report on the pain they feel.
Such vital physiological parameters as HR, BP, RR, oxygen saturation, and EtCO2 are not reliable indicators of pain and can be used only as hints for further assessment of pain with the respective verified methods. When it is acceptable and when a patient cannot say about their sensations, the family can be involved in the evaluation of a patient’s pain [124]. In the pediatric ICU, the simplest pain assessment scales are used starting from the age of 3 years old (Annex 3). At the earlier age, the most significant indicators of pain include crying, face expression, position, and movements of the limbs. The involvement of parents or care givers in the assessment of pain leads to the hyperdiagnostic of pain intensity [123].
Recommendation 35. It is recommended to put on an individual sleep eye mask and earplug for all ICU patients at nighttime in combination with preventive application of drugs for the maintenance of circadian rhythms and prevention of delirium [118, 119, 121]. (level of evidence — 1, grade of recommendation — A).
Comments. ICU conditions, that include constant illumination, personnel talking, monitor alarms, and noise of respirators, inevitably affect the quality of sleep [124]. Meanwhile, the maintenance of sleep in the ICU is a method of decrease in the risk of cognitive impairments, including psychomotor excitement and delirium. Apart from that, the maintenance of the sleep structure provides positive emotional status of the patient, supports their motivation in the therapeutic and rehabilitation program, and increases the tolerance to muscular activity [110].
The pooled analysis of the studies demonstrated a general decrease in the spread of delirium according to the protocol that maintains sleep [124]. In all the studies, the protocols were applied in the management of all ICU patients. An obligatory component of the protocols is the creation of the optimal environment for a patient to provide conditions for normal sleep (natural markers for sleep include window or regulation of light/darkness, refusal from night procedures, regular breaks in the care for 60-90 minutes). To restore the phasal nature of sleep, it is possible to apply Z-drugs. To prevent the disturbances in the circadian nature of sleep, melatonin-containing drugs can be used [120]. Despite the lack of statistically significant approved guidelines on the pharmacotherapy of sleep disorders in ICU patients, there is a list of measures on the sleep maintenance for ICU patients, which showed to be effective [29, 35].
Daytime procedures:
Nighttime procedures:
Wearing of a sleep eye mask and earplugs proved to the most effective devices in the prevention of negative influence in the ICU.
Recommendation 36. It is recommended to switch on music as an element of multisensory impact in the program of cognitive-afferent dissonance prevention for adult ICU patients, including those on CMV [47, 52] (level of evidence — 3, grade of recommendation — B).
Comments. The application of music therapy does not require a specialist in music therapy. It is sufficient to use music fragments of patient’s favorite pieces of music or popular or classic ones. Music contributes to a decrease in the consumption of analgesics [53], reduces the level of anxiety, and increases the adherence to the rehabilitation.
Recommendation 37. It is recommended to follow the protocol for defecation in all ICU patients based on the medical history to prevent circadian rhythm impairments and additional emotional discomfort caused by negative proprioceptive sensations during constipation [111] (level of evidence — 3, grade of recommendation — B).
Comments. Immobilization in a horizontal plane in combination with insufficient (nutritional deficit) or uncommon (tube feeding) are the key reasons for disturbances in the functional intestinal habits, including stereotype and organization of defecation. Underestimation of this topic in the communication with a patient and the formality of the defecation process protocol in the ICU conditions (1 time/2 days) dissimulates the problem relevance but does not decrease its contribution into the development of PICS. Since it is not always possible to establish the premorbid ritual of defecation, it is feasible to prevent constipation with daily defecation unless otherwise specified (abdominal surgery, acute gastroenterological conditions). This issue should be controlled by nurses. Planned administration of laxative suppositories should be made to provide additional anus irritation as an element of defecation modulation.
Recommendation 38. It is recommended to perform training on the restoration of self-care skills for all long-term ICU patients considering the age and cognitive status to prevent routine misadaptation [126, 127, 135] (level of evidence — 3, grade of recommendation — B).
Comments. A separate section in the emotional-cognitive rehabilitation is ergotherapy. In the ICU conditions, ergotherapist trains a patient to perform routine self-care activities (personal hygiene, putting on clothes, taking a meal, alternative or additional communication). The significance of ergotherapy in the structure of RehabICU is in the acceleration of the restoration of premorbid performance patterns of the patient, i.e. a return to habits, life style, and social status.
Including ergotherapy in the rehabilitation complex reduces the time spent in the ICU [127, 135]. In patients with CCS, it reduces the time of adaptation to spontaneous breathing [124], and prevents the development of delirium [135]. In ICU practice, the elements of ergotherapy are included in the responsibilities of nurses and junior medical stuff. But in the future, for the development of RehabICU, a qualified specialist is required.
Recommendation 39. It is recommended to use the Rehabilitation Routing Scale (RRS) for adult patients with PICS (Annex 14) to provide stage-by-stage rehabilitation [38] (level of evidence — 2, grade of recommendation — A).
Recommendation 40. It is recommended to rout all patients with signs of PICS and(or) CCI, RRS score 5-6, to the medical rehabilitation units (MRU) or rehabilitation centers (3–4 levels) with ICU to provide rehabilitation care using the possibilities of telemedical healthcare [128] (level of evidence — 3, grade of recommendation — C).
Comments. Patients, that status of self-care in the routine life did not reach the level sufficient for home care after ICU (RRS 4–6 score), should be directed to local MRU [128] at the place of patient’s permanent residence. Patients with regressing PICS, which does not require hospitalization to MRU (RRS 1-3 score), are provided day-time inpatient rehabilitation or telemedical programs. The volume of rehabilitation program and its rate is determined by the rehabilitation potential of a patient and conditions of state guaranties of obligatory medical insurance valid in the patient’s region of residence. Patients in the state of chronic cognitive impairment (areactive awakening, “minimally conscious state”) after 28 days in the ICU are directed to the respective expert centers of the 3–4 level for the evaluation of the rehabilitation potential and specific rehabilitation).
Criteria for the transfer to the specialized rehabilitation center with ICU for medical rehabilitation of the second stage for patients with PICS or (and) CCI include:
If there are no rehabilitation centers for the organization of telemedicinal service, the application for the telemedical consultation can be sent to the “All-Russian Center of Emergency Medicine “Zashchita” of the Ministry of the Russian Federation”. Requesting the type of consultation, the applicant should specify “chronic cognitive impairment”. RRS score is 6. In the specified day, after a telemedical consultation from the specialists from a certified rehabilitation center, a conclusion should be made to direct the patient for the second stage pf rehabilitation or to a unit of palliative care at the place of residence. The routing of junior children should include a psychologist and a social worker [129].
Recommendation 41. It is recommended to include individual training on how to cope with postoperative psychological and physical prevention of PICS in the program of preparation of patients or parents (care givers) of children for surgical treatment [130–133] (level of evidence — 4, grade of recommendation — C).
Comments. Medical history data on urination and defecation habits (rate and need in stimulation) are important for the organization of postoperative care. It is also necessary to consider somnologic habits (sleep ritual, duration of comfortable sleep) of the patient. Convulsions and other paroxysmal events, constant administration of hypotensive, antidepressant, and hypnotic drugs should be considered. The withdrawal of these drugs can provoke the development of unfavorable events. It is also useful to perform a general evaluation of the level of independence and self-care of patients in the routine life according to RRP scale. The results of primary multidisciplinary examination should be documented in medical documents for further objective evaluation of the dynamics and for legal issues if they arise from the side of a patient or parents (care givers) who are dissatisfied with the treatment outcome.
The preparation for the planned surgery is in the creation of psychological readiness to the limitation of the movement activity and possibility of residual effects of general anesthetic agents. The patient should be trained to apply the methods of compensations and prevention of learned non-use effects. Before the surgery, all members of MDRT examine the patient. After that, an individual program of pre-habilitation is made. The program includes active articular gymnastics in all limbs, stretching of the paralyzed segments with a healthy limb, breathing exercises on the mobilization of a deep diaphragmal inspiration, motor imagery practices that involve the images of movements in the paralyzed limbs (especially, in patients with processes at the spinal level), etc. The communication and education of patients are performed by a clinical psychologist and PRM physician.
The guidelines on anesthesiology can be used as a component of pre-habilitation. It is based on the concept of enhanced recovery after surgery (ERAS). It is an algorithm of anesthesiologic procedures, which includes the optimization of sedative and analgesic components that target their minimally sufficient application. During the early postoperative period, when a patient is available for contacts, MDRT members start individual training of a patient according to the respective methods. Primarily, the program includes active movements in all limbs that are not immobilized. In the immobilized limbs, motor imagery practices are recommended (i.e. imagining or recollecting the limbs movements). An obligatory condition for the start of active movement rehabilitation in the ICU is the lack of absolute contraindications. Simultaneously, specialists start communication with relatives and patient to restore the patient’s memory on preceding events and return the orientation in the place, time, and personality.
Recommendation 42. It is recommended for regional divisions of the Ministry of Health together with territorial funds of medical insurance to issue local acts for step-by-step implementation of RehabICU technology and its adequate financing [38] (level of evidence — 2, grade of recommendation — A).
Comments. According to the Federal Order of organization of rehabilitation care [38] for the realization of RehabICU program, the early rehabilitation units (ERU) should be established. The unit is based on the work of MDRT, which includes a medical rehabilitation specialist (doctor), at least 2 specialists on physical rehabilitation, specialist on ergorehabilitation, medical psychologist/psychotherapist, medical SLT specialist, medical rehabilitation nurse (up to September 1st, 2023 — therapeutic exercise specialist, DPT, reflexologist, therapeutic exercise methodical instructor, medical SLT specialist, physiotherapeutic nurse, massage specialist, and specialist in reflex therapy). The unit is not equipped with beds because its care is provided bedside directly in the ICU. One MDRT provides rehabilitation care to 12 bed in the ICU or 90 post-surgery beds, i.e. the number of NDRT teams is determined by the bed capacity of a medical institution. ERU provides the 1st stage of rehabilitation. After that, the patient is provided with an individual rehabilitation program based on the evaluation of the status of a functional activity according to RRP (Annex 14) [128]. An essential condition of successful implementation of RehabICU is a thoroughly calculated tariff. To evaluate the requirements in RehabICU and financial capacity of obligatory medical insurance budget, the following approach can be used:
The in-house quality control of the provided rehabilitation care is executed according to the approved quality control protocol of the medical institution. Medical-economical expertise is performed by insurance companies according to the common quality criteria (see below) [132].
The following criteria are used for the assessment of medical care quality (Table 4).
Table 4. Criteria for assessing the quality of medical care
| No. | Quality criteria | Level of evidence | Grade of recommendation |
|---|---|---|---|
| 1 | Prevention of PICS syndrome (post-intensive care syndrome) started not later than 48 hours from the moment of the admission to the ICU of a patient of any age. | А | 2 |
| 2 | Daily rehabilitation procedures within RehabICU program ≥ 60 minutes for patients that spent > 48 hours in the ICU. | B | 3 |
| 3 | Rehabilitation manipulations on the mobilization were performed under the control of STOP-signs. Leg raise test was performed before each rehabilitation session. | В | 3 |
| 4 | The evaluation of nutritional status was performed for planning the program of early rehabilitation. | А | 1 |
| 5 | The screening for post-extubation dysphagia was made with a 3-ounce water swallow test. | В | 3 |
| 6 | The expression of the pain syndrome was evaluated daily. | В | 3 |
| 7 | Earplugs and sleep eye mask were used for the prevention of ICU-acquired dyssomnia. | А | 1 |
| 8 | The severity of PICS should be evaluated using PICS-index before a transfer from the ICU. The PICS index was > 10 during a transfer of the patient from the ICU, who spent > 48 hours there. | С | 5 |
| 9 | RRP scale was used for the routing of adult patients with PICS at the stages of rehabilitation. | А | 2 |
| 10 | Early rehabilitation unit was organized in a medical institution with ICU bed fund > 12 beds. | А | 2 |
| Note. The criteria are applied at all three levels of medical care. | |||
The guidelines were developed according to the Decree of the Ministry of Health dated 28.02.2019 No 103n “The approval of the procedure and dates for the development of clinical guidelines, their revision, typical form of clinical recommendations, and requirements to the structure, content, and scientific grounds of the data included in the clinical guidelines” (registered in the Ministry of Justice dated 08.05.2019 No 54588) and the Decree of the Ministry of Health dated 23.06.2020 No 617н “The introduction of changes in Annexes N 1, 2, and 3 to the Decree of the Ministry of Health of the Russia Federation dated 28.02.2019 No 103н “The approval of the procedure and dates for the development of clinical guidelines, their revision, typical form of clinical recommendations, and requirements to the structure, content, and scientific grounds of the data included in the clinical guidelines”.
Disclosure. Belkin A.A. was the Head Scientist in the study “Cytoflavin as a component of rehabilitation therapy for patients with ischemic stroke complicated with PICS syndrome”, funded by the company OJSC “NTF “Polysan”. The other authors declare that they have no competing interests.
Author contribution. All authors according to the ICMJE criteria participated in the development of the concept of the article, obtaining and analyzing factual data, writing and editing the text of the article, checking and approving the text of the article.