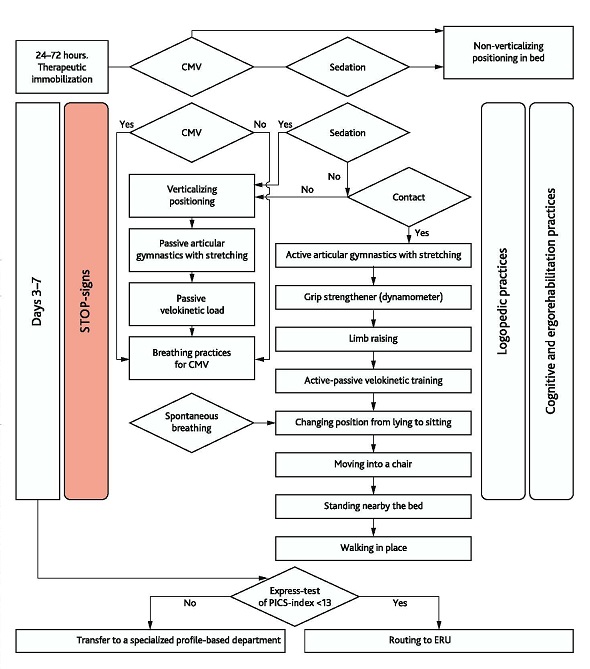
Fig. A1. Algorithms of actions of the anesthesiologist and MDRT
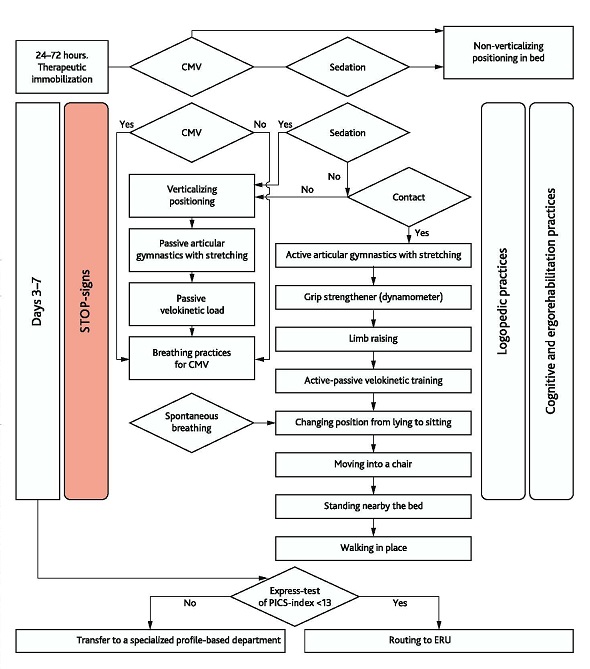
Table A2. Behavioral Pain Scale (BPS) [141]
| 0 | 1 | 2 | Score | |
|---|---|---|---|---|
| Face | Facial muscles are relaxed | Mimic muscles are tense, frowning | Clenched jaws, pain grimace | 0–2 |
| Anxiety | Patient is relaxed, movements are normal | Rare fidget movements, changes body position | Often fidget movements, including head, constant changes of body position | 0–2 |
| Muscular tonus | Normal muscular tonus | Hypersthenia, flexion of fingers and toes | Muscular rigidity | 0–2 |
| Speech | No uncommon sounds | Rare moaning, whimpering, and groaning | Often or constant moaning, crying, quivering, and groaning | 0–2 |
| Rapport, controllability | Calm, cooperative | Can be calmed down verbally, complies with personnel’s instructions | It is difficult it calm down verbally, negative attitude to personnel, does not comply with personnel’s instructions | 0–2 |
| General score: (0–10) | 0-10 | |||
The BPS is not validated in Russia.
Neonatal Infant Pain Scale (NIPS) for newborns/infants to 1 years old is a behavioral tool for the evaluation of pain in undercarried and full-tern newborns.
Table A3. Neonatal Infant Pain Scale (NIPS) [142]
| Parameter | Score 0 | Score 1 | Score 2 | Score |
|---|---|---|---|---|
| Facial expression | Relaxed muscles. Restful face, neutral expression | Grimace. Tight facial muscles, furrowed forehead, brows, chin, and jaw (negative face expression — nose, mouth, brows) | – | |
| Cry* | No cry, quiet | Whimper, mild moaning, intermittent | Vigorous crying, loud scream, shrill, continuous | |
| Breathing pattern | Relaxed, usual pattern for this infant | Visual change in breathing. Irregular air inhalation, faster than usual, gagging, breath holding | – | |
| Arms | Relaxed, no muscular rigidity, occasional random movements of arms | Arms are flexed/extended. Tense, straight arms, rigid and/or rapid extension, flexion. | – | |
| Legs | Relaxed. No muscular rigidity, occasional random movements | Flexed/extended legs. Tense, straight legs. Rigid or rapid extension, flexion. | – | |
| State of Arousal | Sleeping/awake. Quiet, peaceful sleeping with occasional random leg movements | Fussy, alert, restless, and thrashing movements | – | |
| Total Score: | ||||
The intensity of pain is expressed as a total score for each of the six parameters; the minimal score is 0, the maximal possible is 7 (Lawrence et al., 1993). Score > 3 indicates pain. The scale is not validated in Russia.
* Silent crying can be summed if a child is intubated and crying is clear by the movement of mouth and face.
Table A4. Medical Research Council Scale (MRC) [143]
| Score | Muscular Strength | Right arm | Right leg | Left arm | Left leg |
| 0 | No movement is observed | ||||
| 1 | A trace or flicker is palpated in the muscle. Visually — no movement | ||||
| 2 | Movement is possible only when the resistance of the gravity is removed | ||||
| 3 | Movement against gravity is possible | ||||
| 4 | Muscle contraction against gravity and resistance but weaker than on the healthy side | ||||
| 5 | Normal muscular strength |
This scale had various titles. In Russia, it is known as neurological scale of muscular strength.
The pain evaluation is performed by a reanimatologist, ICU nurse, physician (specialist in physical rehabilitation), physical and rehabilitation medicine specialist, neurologist, orthopedic traumatologist.
Conditions of pain evaluation. If the patient is unconscious, objective evaluation is not possible by this scale. If a patient has an expressed cognitive deficit or speaking impairments, it is necessary to monitor the patient and how their limbs move. These data will be used for the evaluation. Besides, alternative sources of communication can be used.
This scale can be used to evaluate the strength of any muscle. The testing of all muscles is based on the principles of manual muscular testing. The specialist should know the position of the tested body and what movement can maximally load the tested muscles. The specialist ensures the antagonist muscles to be excluded from the movement and the tested muscle to be maximally involved in the movement.
Interpreting the obtained data for ICU patients without CNS impairments:
Score 17–20 — no signs of PICS
Score 12–16 — signs of PICS
Score 0–11 — myoplegia or tetraparesis (requires the exclusion of acute CNS pathology)
Tobin Index [27] is an index of rapid shallow breathing (RSBI). RSBI parameter is calculated by the formula:
RSBI = f/Vt,
where in f is the respiratory rate (per minute); Vt — breathing capacity (L).
During the calculation of RSBI, the patients breathes without additional help or during ventilation with minimal pressure (< 5 cm H2O) and the doctor measures the breathing volume and RR of the patient. This evaluation is performed with no mechanical help from CMV or other equipment to the patient. The normal Tobin Index is < 105 breaths/min/L. If RSBI is < 100, the patient can be extubated, the possibility of successful transfer to spontaneous breathing without complications is 80–95 %. If RSBI > 120, the patient will need further respiratory support and the diagnosis of ICU-acquired weakness can be established.

Original name: In Russian: “индекс мобильности Ривермид”. In the Russian Federation, the scale is not validated.
Rivermead Mobility Index is a simple and available test that evaluates not only walking but also patient’s mobility. To be applied in ICU, the index was modified several times (F.M. Collen et al., 1991; D. Wade, 1992, C. Hodgson, 2014; А.А. Belkina, 2014).
Table A7. Modified Rivermead Mobility Index (mRMI-ICU) [144]
| Level | Skill | Description | Result |
|---|---|---|---|
| 0 | Immobile in bed | A patient is not able to change the position in bed. The patient is passively mobilized by medical personnel. | P |
| 1 | Active in the bed | A patient can turn from the back to a side without assistance, cyclic kinesiotraining, exercises with assistance. Patient cannot get out of the bed without help. | P |
| 2 | Passive sitting up without keeping balance | A patient can be transferred to a sitting position in the bed or chair with back support with an elevator or personnel assistance. The patient cannot sit on the edge of the bed. | P |
| 3 | Active-passive sitting up on the edge of the bed with balance keeping | A patient can sit up from a lying position on the edge of the bed and keep balance for 10 seconds with or without assistance. | P |
| 4 | Changing position from sitting to standing | A patient can stand up and keep standing with the help of hands, stander, or tilt-table | P |
| 5 | Transfer | A patient can be transferred from the bed into a chair and back with assistance. | P |
| 6 | Walking in place | A patient can lift each leg 2 times and transfer the center of gravity on the opposite leg. | P |
| 7 | Walking | A patient can make 2 steps with a high walker or bilateral assistance. | P |
Comment. mRMI-ICU value corresponds to the score of doctor’s positive assessment of the patient on each parameter.
Interpretation. The index can score from 0 (inability to make any movements) to 15 (ability to run 10 m). In the modification proposed for ICU patients, the normal score is 7.
Hodkinson’s Mental Abilities Test — 10 (AMT-10) is used to assess three cognitive domains. Each correct answer scores 1. The threshold score is ≤ 6. Questions 2–6 are asked to assess the patient’s orientation in time, place, and personality. Questions 1, 7–9 are asked for the assessment of memory and general level of knowledge. Question 10 (and 1) is asked for the assessment of attention.
Table A8. Hodkinson’s Mental Abilities Express Test [145]
| Question | Score |
|---|---|
| Patient’s age | 1 |
| Date and year of birth | 1 |
| Time of the day (approximately) | 1 |
| Current date (day, month, year) | 1 |
| Current place (hospital, department) | 1 |
| Current time of the year | 1 |
| Name of the wife (husband, children) | 1 |
| Name of the President | 1 |
| Repeat the doctor’s name (Doctor needs to introduce themselves first) | 1 |
| To count down from 10 (corrections are acceptable if they are made by the patient themselves) | 1 |
Score 10 is a norm (1 point for each question).
Table A9. Criteria for calculating the PICS index [43, 44]
| No. | Modality of Symptoms | Type | Score |
|---|---|---|---|
| 1 | Infectious and trophic complications | Decubitus | 0.5 |
| Respiratory tract infection | 0.5 | ||
| Urological infection | 0.5 | ||
| 2 | Vegetative and metabolic complications | Pain, diencephalic crisis | 1.0 |
| Circadian rhythm impairment: dyssomnia | 0.5 | ||
| Decrease in the gravitational gradient | 1.0 | ||
| Decrease in the load tolerance | 0.5 | ||
| Nutritional deficit | 1.0 | ||
| Body mass deficit | |||
| 3 | Neuromuscular complications | ICU-acquired weakness | 1.0 |
| Respiratory ICU-acquired weakness | 0.5 | ||
| ICU-acquired dysphagia (learned non-use) | 1.0 | ||
| 4 | Emotional and cognitive complications | Memory and orientation impairments | 0.5 |
| Delirium/Hallucinations | 1.0 | ||
| Depression | 0.5 | ||
| TOTAL | 10.0 |
Note. Gradation of PICS index by the degree of severity:
Score 1–3 — mild.
Score 4–6 — moderate.
Score 6–10 — severe.
PICS Index Express Test is used by a reanimatologist-anesthesiologist during a transfer of a patient from ICU to a specialized department.
Table A10. Criteria for calculating the express PICS index
| Criteria | Norm | Mild | Moderate | Severe |
|---|---|---|---|---|
| Mobility (Rivermead Scale) | 7 | 5–6 | 3–4 | 0–2 |
| Cognitive status (Hodkinson’s Scale) | 10 | 8–9 | 4–7 | 0–3 |
| PICS index gradation | 17 | 13–16 | 6–12 | 0–5 |
Instruction:
Note. The index is not calculated for patients with acute cerebrovascular insufficiency of any genesis. The PICS index interpretation should include the data on the premorbid mobile and cognitive status of the patient.
Table A11. The nomenclature of basic and adjuvant techniques used by MDRT in ICU
| No. | Name | Classificator | Code | Description | Dosing Regimen | ||||
|---|---|---|---|---|---|---|---|---|---|
| 1. | Positioning (Full version of the protocol at: http://rehabrus.ru/index.php?id=55) | ||||||||
| Horizontal (non-verticalizing) | A14.30.001 | П0 | Lying on the back Lying on a healthy side Lying on a lesion side Prone position |
Day 1 for patients with shock and/or in the premorbid phase of acute cerebrovascular insufficiency (ACI) Change of the position not rarer than every 2 hours according to the local protocol |
|||||
| Verticalization | A23.30.017 | П1 | Lying on the back on an elevated head bed end at 30–45° (Fowler’s position) | From Day 1, basic position with interruptions for sleep and other rehabilitation measures considering subjective tolerability or STOP-signs | |||||
| П2 | Semi-recumbent position (the elevation of the bed head is 45–60°, in the bed) | During taking a meal, considering tolerability | |||||||
| П3 | Semi-sitting position (the bed head elevation is 67° ± 5°), the bed leg end is lowered | When П2 is achieved, this position should the used as the main one for the preparation of moving to a chair 30 minutes × 2 times per day The beginning and duration depend on the tolerability of a patient and lack of STOP-signs From 5 minutes × 2 times per day The step of gradual increase in the duration is 10 minutes |
|||||||
| П4 | Sitting position on the bed with legs down with and without support, keeping balance to strengthen back muscles, or sitting in a chair | To start after the achievement of 1-hour tolerability of stage M2 The rest conditions are the same. It is suitable for patients with chronic cognitive impairments because it is impossible to for such patients to sit on the bed edge. It accelerates the process of adaptation to the chair. |
|||||||
| П5 | Standing position | The patient should stand and keep balance with assistance or using additional equipment (Clinical Guidelines on verticalization at: http://rehabrus.ru/index.php?id=55) Keeping balance standing in a stander, with assistance, using a system of weight distribution or simultaneously Sifting from foot to foot for 30 seconds nearby the bed. Start after the achievement of 1-hour tolerability of the step M3. The rest procedures are the same |
|||||||
| 2. | Transposition | ||||||||
| Passive | A14.30.001 | М0 | Changes in the positioning using a configuration of the bed, verticalization table, winch | ||||||
| Assisted | A19.23.002.014 | М1 | Changes of the positioning with assistance of 1–2 people or special equipment (stander, system of weight distribution). The transfer is made passively with an elevator or passively-actively with a stander or assistant, transfer into a mobile or bedside chair. | ||||||
| Unassisted | A14.30.016.1 | М2 | Unassisted change in the positioning (turning in bed, sitting up, transfer to a chair, standing up) using supporting surfaces (chair back, cane, walker) | ||||||
| 3. | Mobilization | ||||||||
| Verticalization | A17.02.002 | В | Diagnostic and training procedure of the controlled change of the elevation angle of the head bed end using special equipment (electric verticalizators, FES) for the assessment of gravitational gradient and orthostatic training. | Full version of the protocol at: http://rehabrus.ru/index.php?id=55 An increase in the angle of elevation of the head bed end with further lowering of the leg bed end with 1–3 assistants:
|
|||||
| Passive Kinesiotherapy | A19.23.005 | К0 | Passive movements in joints in the volume of physiological limits without stretching | From Day 1, 10 slow movements in each joint.The duration of 1 session is 20 mins.Joints:
|
|||||
| A19.23.001 | К1 | Passive movements in joints in the volume of physiological limits with muscle stretching | |||||||
| A19.23.002.025 | Monoarticular training aid (intended for training of separate joints: knee, pelvis, ankle, hand, shoulder). The same exercises using mechanical training aid (including, robotized) that provides cyclic training for separate joints and has sensors for the assessment of the patient’s impact in an active-passive mode (if indicated during post-operative or post-traumatic immobilization of 1 limb). |
From Day 2, 20 mins × 2 times a day | |||||||
| Active Kinesiotherapy | A19.23.001 | К2 | Active articular gymnastics with stretching: scapula elevation/inversion pelvis elevation/inversion body twisting head turning, flexion and extension shoulder flexion/extension, adduction/abduction, internal rotation/external rotation forearm flexion/tension, pronation/supination hand flexion/extension, adduction/abduction finger flexion/extension, spreading, opposing thigh flexion/extension, adduction/abduction, internal rotation/external rotation knee flexion/extension feet flexion/extension, internal rotation/external rotation complex movements with one or several limbs |
Step 1 — overcoming of the resistance of gravity by lifting and keeping a limb up to 10–30 seconds Step 2 — active single movements with attempts to be repeated up to 8–12 times Step 3 — increase in the number of series up to 3 Step 4 — increase in the intensity up to 11–13 by Borg scale Step 4 — increase in the number up to 2 per day Along with an increase in the tolerability from 5 to 20 mins × 2 times per day |
|||||
| A19.23.002.017 | К3 | The same movements but with overcoming the resistance created by the instructor or elastic belt. It is possible to apply a grip strengthener or ergometer | |||||||
| A19.30.014 | К4 | Walking in place | |||||||
| A14.30.018.2 | К5 | Walking around the bed or with assisting equipment (high walker, weight distribution frame) | |||||||
| 4. | Cyclic Loads | ||||||||
| Passive velokinesis | A23.30.023 | TS0 | Veloergometer for lower and (or) upper limbs (obligatory for patients on CMV) | 20 min × 20 cycles/min | |||||
| Active velokinesis | A12.10.005 | TS1 | Veloergometer for lower and (or) upper limbs | 10–30 min × 2 times, from Day 5–7 of CMV, 20 mins × 2 times/day | |||||
| 5. | ADJUVANT modulations of kinesiotherapy | ||||||||
| Neuromuscular electrostimulation | A17.24.010 | F1 | Neuromuscular stimulation of muscular contractions as a sensory irritation and preparation for mobilization using a portative electrostimulator | From Day 2, daily × 1 time/60 mins, 45 Hz | |||||
| A17.24.011 | F2 | In patients on CMV, intercostal muscles and diaphragm should be stimulated | Daily × 1 time/50 mins | ||||||
| Pneumocompression of lower limbs | A15.12.002.001 | F3 | Prevention of deep vein thrombosis at all stages, including pre-mobilization | ||||||
| 6. | RESPIRATORY REHABILITATION (PREVENTION OF MUCOCILIARY CLEARANCE IMPAIRMENTS) | ||||||||
| Extrapulmonary mechanical stimulation | A19.09.002 | Р1 | Percussive manual massage of the thorax before sanitation | From Day 1, 5–6 times/day, 3–5 mins each time | |||||
| A21.12.002 | Р2 | High frequency chest wall oscillation (VEST) | From Day 2, the procedure is performed in a semi-sitting position of the patient with a 30–40° elevated head bed end Parameters (frequency — 10–15 Hz; pressure 5–10 mmHg) 5–6 times per day, 10 mins each time |
||||||
| A19.09.001.001 | Р3 | Active breathing gymnastics (cooperative patient) focused on the involvement of the diagram | From Day 1, 5–6 times/day, 5–7 sets each time | ||||||
| Active maneuvers with the application of respiratory exerciser | A19.08.001 | Р4 | Cycles of spontaneous breathing positive end expiratory pressure (PEEP) (speaking valve, stimulating training equipment for inhale/exhale) to preserve vital lung capacity, effective cough impulse, and phonation | 5–10 mins × 2 times/day | |||||
| Aerosol therapy | A17.09.002.001 | Р5 | Inhalations with drugs to affect the sputum properties for its easy evacuation | When indicated | |||||
| 7. | Logopedic complex RehabICU | ||||||||
| Prevention of post-extubation dysphagia | A19.23.002.010 | L1 | Logopedic massage and articulatory gymnastics | During massage, stimulation of mucous membranes in the oral cavity, including taste receptors. Cooperative patients are offered to take active part during the exercises | |||||
| A14.30.003 | L2 | Food consumption training by SLP specialist (VVT-test) | Food consumption training is performed with VVT-test, which is a safe consistence of bolus in terms of the risk of aspiration | ||||||
| 8. | Complex of clinical psychology and ergotherapy RehabICU | ||||||||
| Prevention of emotional-cognitive impairments | A21.23.005 | E0 | Sleep hygiene (sleep eye mask, earplugs) | At night, the patient is offered to use a sleep eye mask and earplugs, which is useful for the maintenance of common night sleep habits | |||||
| A13.29.020 | E1 | Cognitive abilities: place, time, personality, reading | Clinical psychologist MDRT or ICU personnel assess the level of orientation of the patient in the current situation every day for 2–3 minutes × 2 times. If cognitive, amnestic, or emotional problems are revealed, a clinical psychologist is called for thorough testing and treatment. | ||||||
| A13.29.007.004 | E2 | Music therapy | For 30 mins × 2 times/day or on request, the patient is offered to listen to the music chosen by a clinical psychologist, which includes classical and popular melodies | ||||||
| A21.30.006 | E3 | Skills: spoon, remote controller, tooth brush, call button, putting on clothes | During the exercises, the patient is offered to apply routine skills themselves or with the help of ergotherapists for 20 mins × 1 time/day | ||||||
| A21.23.006 | E4 | Communication with relatives | The patient can communicate with relatives for 20–30 minutes. Positive topics for discussion and tactile expression of emotional support (hugs, kisses), relaxing massage (for example, massage of the heel area) | ||||||
Absolute contraindications to the beginning of mobilization:
Relative contraindications to the beginning of mobilization:
Table A12. Dynamic STOP-signs
| No. | Section of Monitoring | Range of values | Method of Registration | Contraindications to the beginning or STOP-signs during the procedures |
|---|---|---|---|---|
| Obligatory Modalities | ||||
| 1 | Volume status | Negative PLR-test | Clinical test | Positive PLR-test [56,57] |
| 2 | Systolic blood pressure (SBP) | > 90; < 180 [2] mmHg > 90; < 200 [1–3] |
Non-invasive (invasive if indicated for the primary disease) Apparatus monitoring | Decrease in SBP by > 20 mmHg or 20 % from the baseline [48, 49] SBP <100 or > 180 within > 3 mins of manipulations [137] |
| 3 | Diastolic blood pressure (DBP) | > 50; < 110 mmHg | Decrease in DBP by 10 mmHg or 20 % [136] from the baseline within > 3 mins DAD <50 or >110 [137] |
|
| 4 | Mean BP (mBP) | > 60 mmHg < 110 mmHg [1] | mBP < 60 or >110 [49, 137] Decrease in mBP by 15 mmHg |
|
| 5 | Central hemodynamics | No signs of acute coronary syndrome [1] | ECG monitoring | Depression of ST segment (> 2 mm) with normal resting ECG Elevation of ST segment (> 1 mm) in the leads without pathological Q wave (except V1 or AVR) Negative or increasing T [137] |
| 6 | Cardiac rhythm | Sinus rhythm [1] or permanent atrial fibrillation | Acute development of arrhythmia [48, 137] His bundle branch block, especially if it is not distinguishable from ventricular tachycardia (“wide QRS tachycardia”) Increase in ventricular extrasystole, especially, if it exceeds 30 % from sinus complexes |
|
| 7 | Heart Rate (HR) | > 50; < 130 per min [1, 10] | Non-invasive apparatus or clinical monitoring | < 60 or > 130 within 3 mins [48, 137] or increase in the HH by 20 % [20, 49, 136] |
| 8 | Pharmacological maintenance of hemodynamics | Dopamine < 10 µg/kg/min Noradrenalin < 0.1 µg/kg/min |
Increase in the dose of adequate hemodynamic supply within 3 mins after the beginning of the procedure [20, 137] | |
| 9 | Blood saturation (SpO2) | > 90 % | Pulseoxymeter | < 90 % decrease in desaturation by 4 % [47–49], 5 % [136], and more from the base line within 3 mins [137] |
| 10 | Level of consciousness or sedation | Scale of sedation RASS = [–5; 2]. Condition of the patient that does not require indication of additional sedation and (or) neurolepsy (“quiet patient”) |
Clinical monitoring or BIS (ECG)- monitoring | RASS < –3 or > 2 [20, 137] Decrease in the level of consciousness by 1 and more than 2 points [47] Increase in the requirement in sedation (including for synchronization with CMV apparatus) Seizure activity Psychomotor excitement |
| 11 | Pain Status | 0 by BPS or VAS scale | Clinical monitoring | Appearance or intensification of pain [137] |
| 12 | Respiratory Rate (RR) | > 10; < 40 > 5; < 40 [1, 10] |
Non-invasive apparatus or clinical monitoring | bradypnea or tachypnea [20, 48] dyspnea and hissing respiration |
| 13 | Axillary temperature | > 36.0; < 38.5 °C | Thermometry | < 36.0 or > 38.5 [20, 47, 137] |
| 14 | Borg Dyspnea Index | < 11–13 > | Clinical monitoring | Borg Dyspnea Index > 13 [20] |
| 15 | Vegetative nervous system status | No clinical signs of dysfunction | Clinical control | Acute dysautonomia paroxysm: hyperhidrosis, tachycardia, hyperthermia, muscular hypertonus, paleness, weakness [20, 138] |
| Additional modalities for patients on CMV | ||||
| 1 | Synchronicity with CMV | Synchronicity | Clinical observation | Desynchronization |
| 2 | Content of oxygen in the in the inhaled air (FiO2) | < 60 % | Gas analyzer of CMV apparatus | Increase in the consumption of oxygen [20, 47, 48] |
| Respiratory index PaO2/FiO2 | < 300 — acute lung injury, < 200 — acute respiratory distress syndrome Norm 500 (PaO2 : FiO2 = 100 mmHg/0.21 = 476) [139] |
Gas analyzer | Any decrease in the respiratory index | |
| 4 | Partial pressure of CO2 in the arterial blood (PaCO2) | < 60 mmHg | Gas analyzer | Increase of hypercapnia |
| З | Positive end expiratory pressure (РЕЕР) | <10 cm H2O | Monitor of CMV apparatus | Increase in РЕЕР [47, 48] |
PLR (passive leg raising test) is a test based on leg raising for the assessment of the volume status [56, 57].
Physiologically, the test is based on the involvement of the patient’s blood volume (autotransfusion). This test precisely predicts an increase in the cardiac output of the blood from the lower limb veins to the right sections of the heart, which is around 300 ml.
The peculiarity of this test is in its absolute reversibility and possibility to be performed both in patients with preserved spontaneous breathing and those that are on CMV. There are no contraindications to PLR test in patients with heart rhythm disorders as well as during inotropic and/or vasopressor support.
Method: stretched out legs are raised to at least 600 in a patient who is horizontally lying on the back. The parameters of hemodynamic (BP, HR, central venous pressure) are registered before the raising and in the highest point.
The test is positive if there is an increase in BP and (or) HR by 10 %, CVP — by 2 mmHg from the initial level. Positive test is a contraindication for the start of RehabICU (detailed information at https://rehabrus.ru/Docs/2021/MR-ReabIT_3.0.pdf).
Table A14. Gradations of The Rehabilitation Routing Scale (version for ICU) [5, 128]
| RRS parameters (score) | Description of functioning and limitation of vital activity | Routing |
|---|---|---|
| 0 | No functional impairments and limitations of vital activity — functions and structures of the organism are preserved in full | Not indicated |
| 1 | No manifestations of functional impairments and limitations of vital activity in patients with symptoms:
|
Not indicated |
| 2 | Mild impairment of the functioning and limitation of vital activity — can live alone at home from a week and more without additional help:
|
Not indicated |
| 3 | Moderate impairment of functioning and limitation of vital activity — can live alone at home without additional help from 1 day to 1 week:
|
Course of medical rehabilitation with the application of telemedicine technology with further hospitalization to a day-time inpatient facility according to a waiting list and epidemiologic situation. |
| 4 | Manifested impairment of functioning and limitation of vital activity — can live without assistance up to 1 day:
|
Routing to the 2nd stage of medical rehabilitation to the department of inpatient medical rehabilitation with further rehabilitation at the 3rd stage (recreational-balneologic institution) using telemedicine technology |
| 5 | Severe impairment of functioning and limitation of vital activity:
|
|
| 6 | Extreme impairment of functioning and limitation of vital activity:
|
Routing to the ICU for the 2nd stage of rehabilitation with further individual routing |