Hemodynamic stability is a treatment target in the pediatric critical care. The main therapeutic way of providing is infusion therapy (IT) [1–4]. The issues of the qualitative and quantitative composition of infusion programs, safe methods of administration, and a comprehensive assessment of the effectiveness of intravenous solutions in the near and long term remain are debating [1, 2]. In intensive care units (ICU) volume overload remains high in the first days [1, 3]. The priority of a restrictive IT strategy aimed at reducing mortality and complications is considered by modern reviews [2, 3]. In young children, hemodynamic regulatory mechanisms are imperfect and determine a high risk of rapid maladaptation and decompensation of the pathological process [5, 6]. There are features of cardiac activity in newborns: low catecholamine sensitivity, poor development of beta adrenergic receptors, the predominance of adrenergic mechanisms over cholinergic ones, the baroreflex immaturity. Newborns have a higher total body water and extracellular compartment with greater sensitivity to fluid dynamics and rapid movement compared to adults. Severe dehydration may be complicated by hypovolemia, decreased cardiac output and shock, especially in preterm infants. Excess volume infusion is considered unpredictable [7, 8]. Intraoperative intravenous fluid administration has some peculiarities in children under regional anesthesia. According to a comparative analysis [9] in children of the younger (1–5 years) and older (6–12 years) age groups, it was found that a typical hemodynamic response to an epidural block is a slight decrease in peripheral vascular resistance and blood pressure without a significant change in cardiac output in older children, but successfully corrected by emergency rehydration. Rarely hypotension accompanies epidural blocks in newborns and young children, so a volume preload reducers [10]. Hemodynamic stability is explained by the autonomic sympathetic immaturity, a lower peripheral vascular resistance and a smaller blood volume deposited in the lower extremities [8, 11, 12].
Non-invasive monitoring of vital signs does not allow unambiguous interpretation of in hemodynamic changes; invasive control methods are limited in children. Studies of heart rate variability as an indicator of the body's autonomic response to stress factors (pain, trauma, psycho-emotional overstrain, hypo-, hypervolemia, infectious process) are relevant. The possibility of cardiointervalogram data for dynamic monitoring of the effectiveness of drug therapy in critically ill patients is considered as a method of intra- and postoperative control in different age [13, 14].
Objectives. To study the features of the electrophysiological response to the emergency rehydrate volume in children upon admission to the intensive care unit.
A prospective comparative study was carried out in the children's intensive care unit of the Novosibirsk State Regional Clinical Hospital. The study was approved by the local ethics committee of the Novosibirsk State Regional Clinical Hospital, (Protocol No. 1, dated 2021/03/09). Inclusion criteria: patients aged from 1 day to 15 years for the first two hours from the moment of admission the ICU, of a somatic or surgical pathology, provision of the postoperative period under conditions of regional anesthesia.
The children were divided into two groups according to age, and each of them into two subgroups depending on the surgical intervention.
The first group enrolled newborns (n = 71), in 30 % surgical cases (n = 21), with epidural analgesia (EA) with ropivacaine 0.2 % infusion 0.2 mg/kg/h in the early postoperative period. According to nosology: high intestinal obstruction — 55 %, low — 30 %, gastroschisis — 15 %. Newborns (n = 50) had somatic pathology with organ disorder in the early neonatal period with infection: pneumonia, enterocolitis stage II a-b according to Walsh and Kliegman (1987)) — 47 %; asphyxia — 16 %, jaundice — 14 %, hemorrhagic disease — 6 %, others — 17 %.
The age and body weight were comparable in both groups: somatic — 7 days [5; 20] and surgical — 7 days [4; 13] (p = 0.64), body weight 2.96 [2.53; 3.35] and 2.72 [2.2; 3.38] (p = 0.73). More than 70 % of newborns had a length of gestation over 36 weeks. More than 70 % infants were born over 36 weeks' gestation.
The second group (n = 101) enrolled children aged 1 to 15 years, in 40 % surgical cases (n = 41), with epidural analgesia with ropivacaine 0.2 % infusion 0.4 mg/kg/h in the early postoperative period. Surgical pathology included intestinal obstruction — 10 %, complicated appendicitis — 15 %, abdominal, retroperitoneal and pelvic tumors — 29 %, intestinal strangulation — 12 %, orthopedic pathology — 24 %, other (urology, gynecology) — 10 %.
The study of the vegetative status was carried out by the cardiointervalography (CIG) — a complex for wireless monitoring of electrophysiological signals «Callibri» (Neurotech, Taganrog, RF). Data collecting was performed by the screening survey of short-term periodic variations [6]. A sample of 500 RR intervals during a 5–10 minute at patient rest were analyzed. Registration of CIG parameters in all subjects was performed in the first two hours upon admission: before emergency rehydration with balanced crystalloid solution (Sterofundin ISO) 10 ml/kg/h (stage 1), immediately after the infusion (stage 2). Indications for rehydrate in somatic children were clinical and laboratory signs: tachycardia, decreased urine volume, dry mouth, thirst in older children, weight loss, high hematocrit. In the surgical group, intravenous therapy, corrected of pathological losses mainly through the gastrointestinal tract (GIT), continued in the postoperative period in order to avoid volume overload of the pulmonary circulation. Fluid losses were explained by intestinal paresis, evacuation disorders (vomiting, intestine regurgitation). Sevoflurane was used as induction to 1.0 % maintenance concentration during the operation, fentanyl at doses of 5 to 8 mcg/kg/h, an additional sensory block by epidural analgesia with ropivacaine 0.2 % infusion 0.2 mg/kg/h — 0.4 mg/kg/h (depending on age) in all cases. The volume of intraoperative infusion was 10 ml/kg/h of saline.
Non-invasive hemodynamic parameters: heart rate (HR); mean arterial pressure (MAP); CIG parameters: stress index (SI), indicator of activity of regulatory processes (IARP); the proportion of the most common cardio interval (аMo); spectrum powers: the power of the spectrum of the very low-frequency component (VLF), the power of the spectrum of the low-frequency component (LF), the power of the spectrum of the high-frequency component (HF), centralization index (IC, IC = (HF+LF)/VLF)) were included in study.
The data with the normal distribution law (Shapiro–Wilks criterion) were described as median (Me), lower (Q25) and upper (Q75) quartiles. The Mann–Whitney test was used for intergroup comparisons of quantitative variables; the Wilcoxon test was used in the inter-stage comparison. A p-value of < 0.05 is the statistical significance.
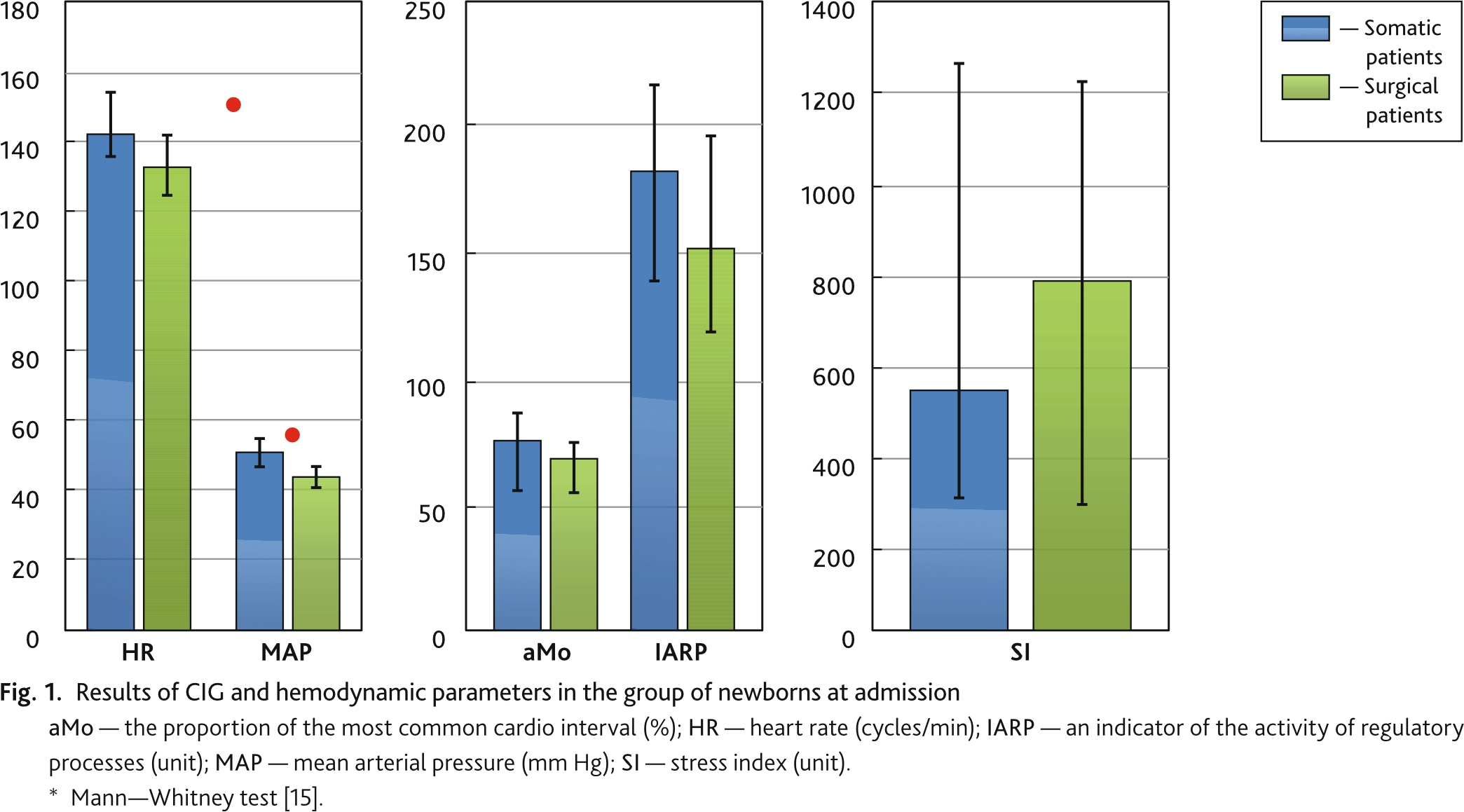
Statistical and frequency of the cardiointervalogram’s data in newborns at the 1st stage of the study did not differ significantly in the intergroup comparison (Fig. 1).
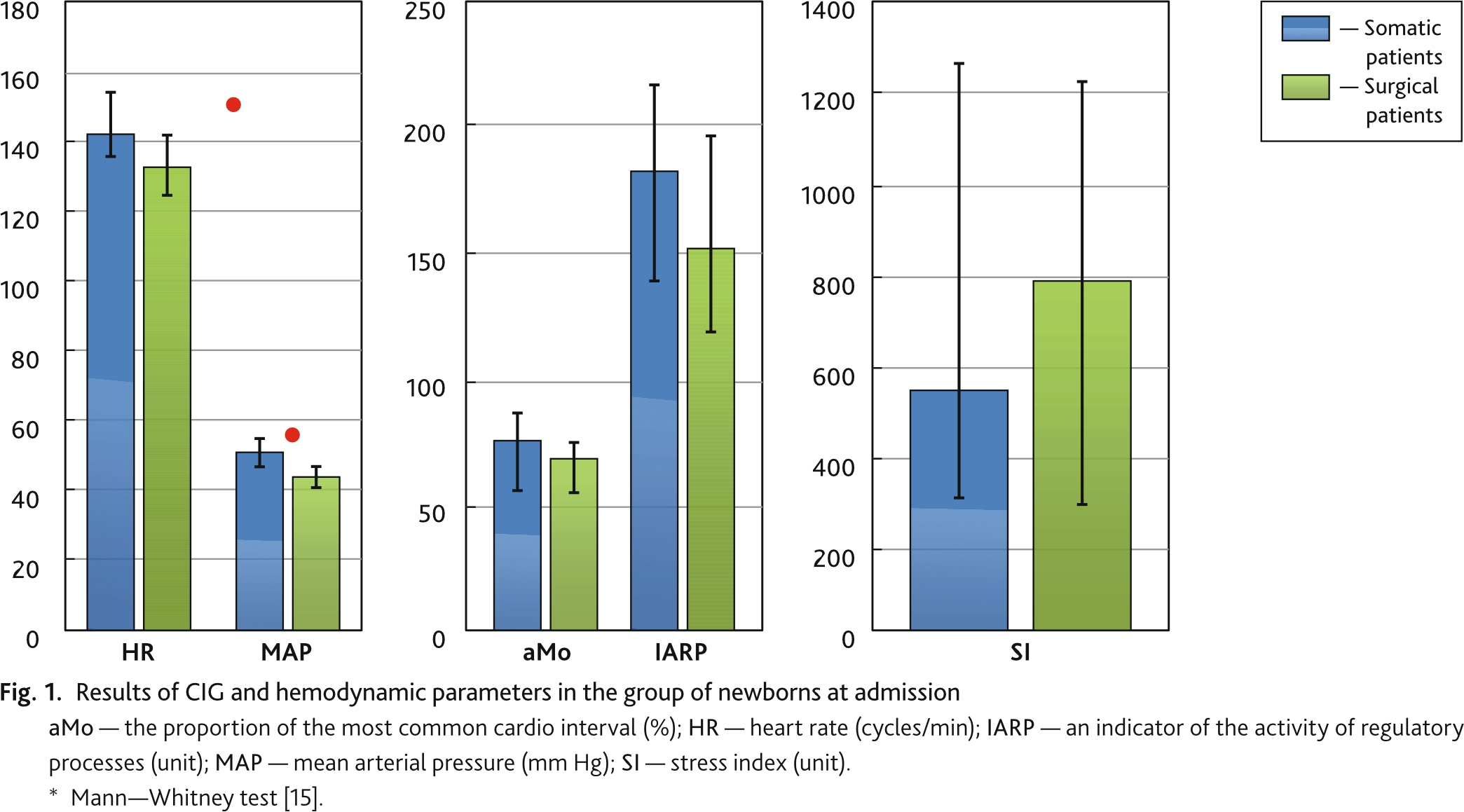
The difference between heart rate and MAP was statistically confirmed (p = 0.009 and p = 0.000, respectively), but the difference was within the age range. The high level of sympathicotonia and the dominance of the central regulation of the heart rhythm were determined initially. The action of triggers (surgical trauma, initial pain syndrome, risk of disruption of adaptation processes) was characterized by a non-specific picture of tension in the regulatory response of the autonomic nervous system. A significant difference in all indicators was revealed in children at the 1st stage of the study (Fig. 2).
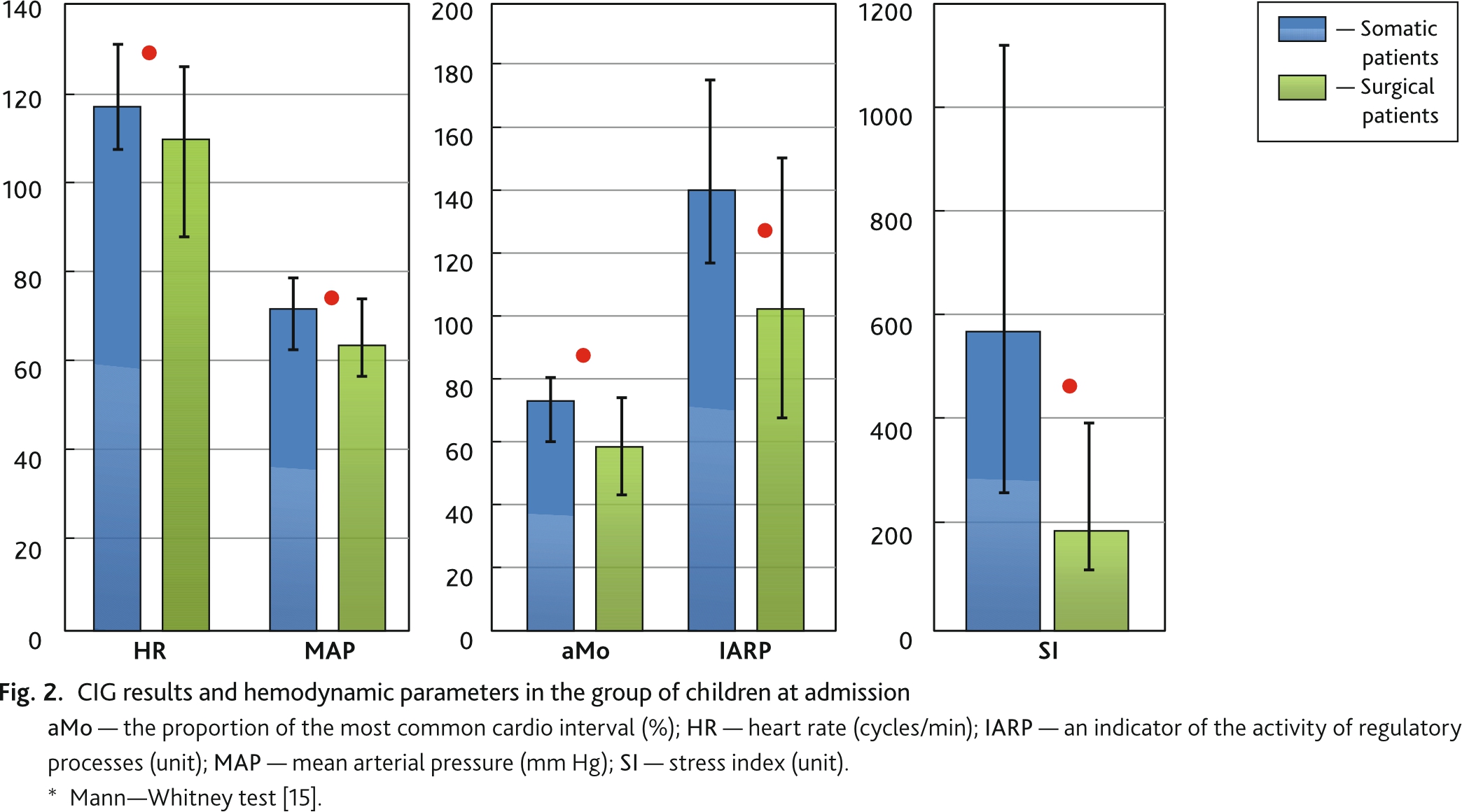
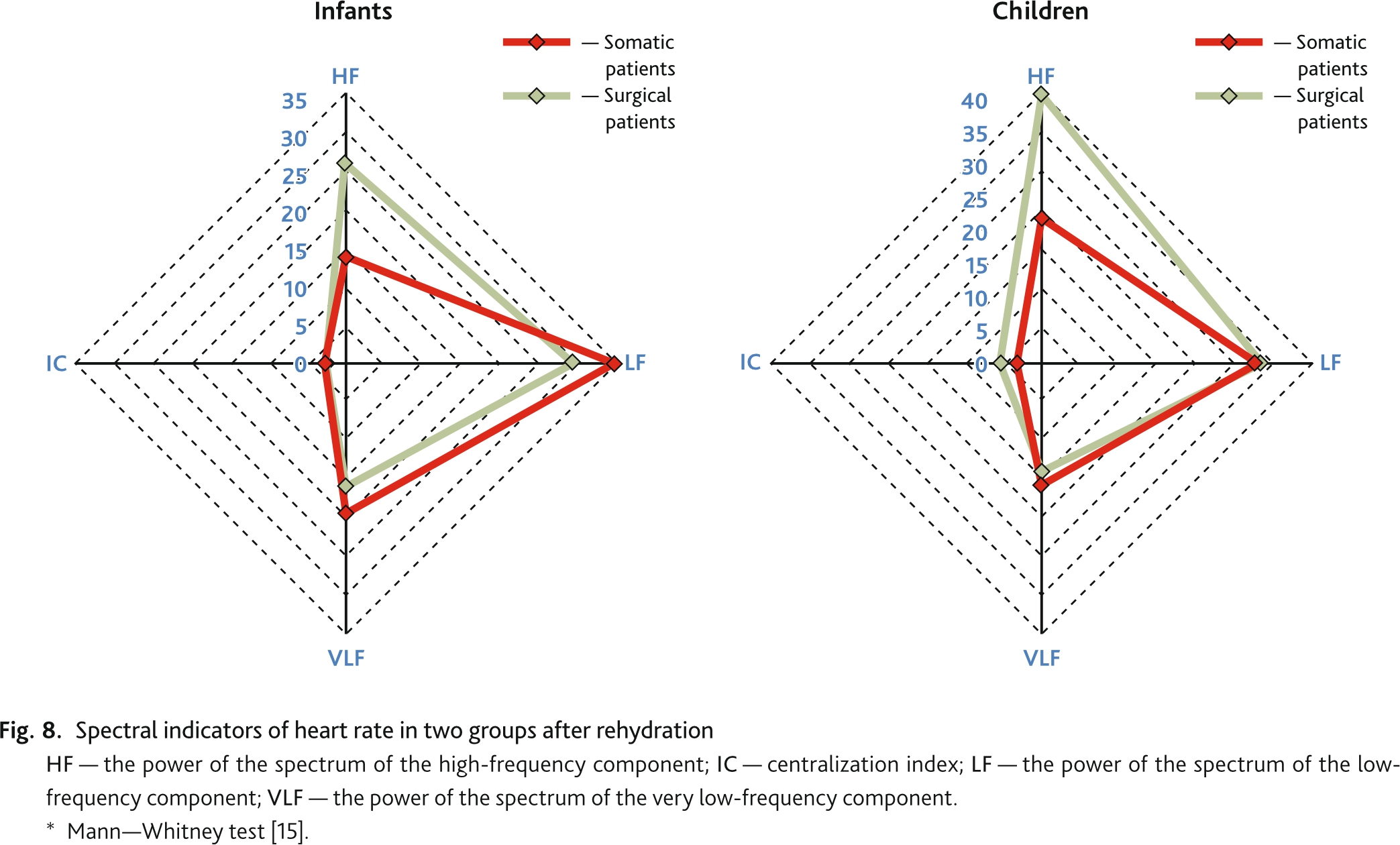
Overstrain of regulatory systems was noted in children with somatic pathology. The predominance of central regulatory mechanisms over autonomous ones was explained by the failure of adaptation and age awareness of the situation. Indicators of the activity of the sympathetic division were significantly lower in children in the early postoperative period due to the residual effect of general anesthesia. The comparability of the normal proportion of low frequency spectral waves (LF) were characterized the satisfactory state of the vascular tone regulation system in two subgroups (Fig. 3). The indicator of vagal activity (HF) was relatively suppressed in the surgical group.
The ratio of low frequency waves was characterized the satisfactory state of the vascular tone regulation system in two subgroups. The range of volumetric regulation oscillator (HF) was significantly pronounced in children after surgery (p = 0.000). The increase in the overall spectrum due to HF overload determined a significant increase in IC with a decrease in VLF. In newborns, activity and frequency ratio did not differ significantly.
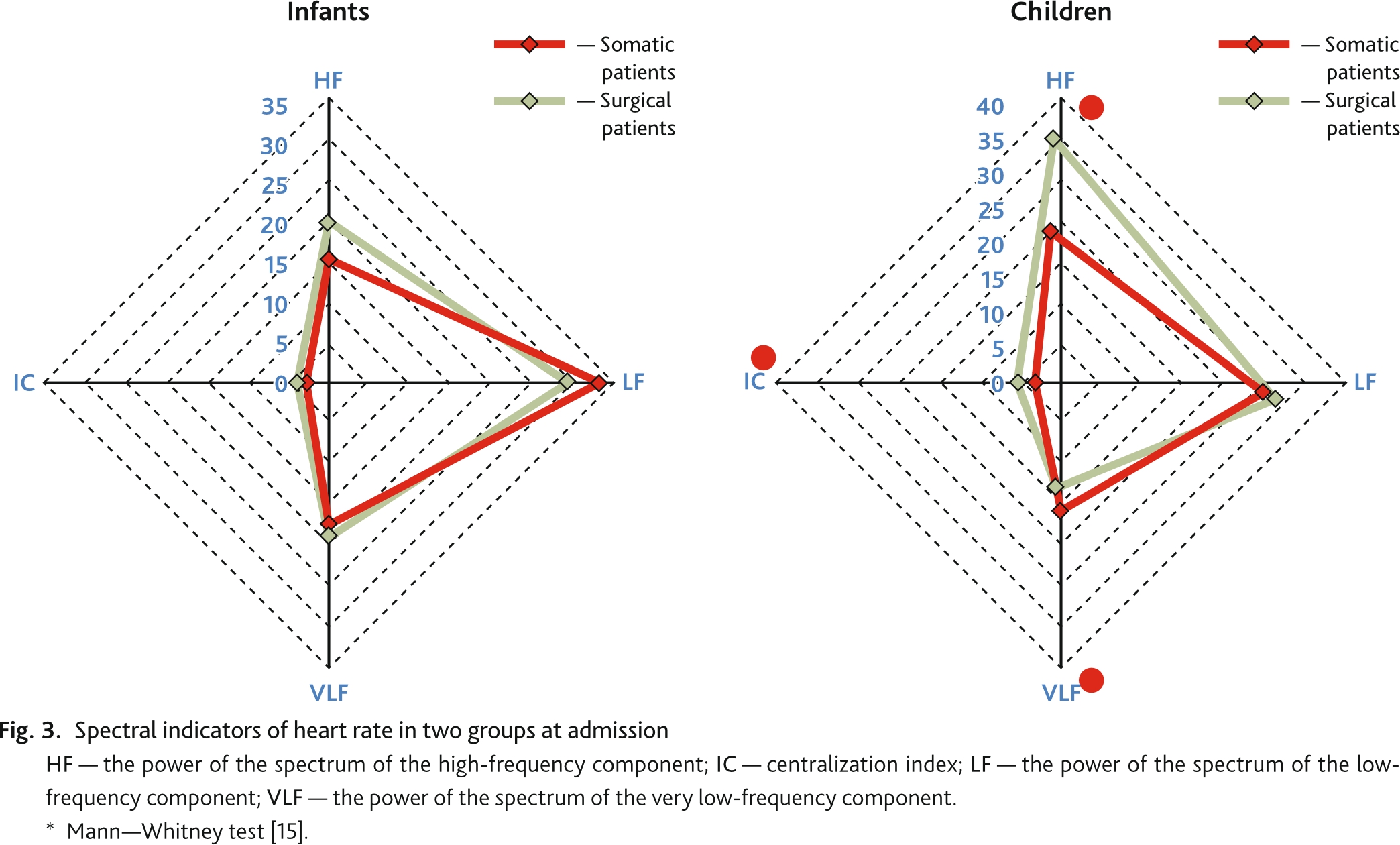
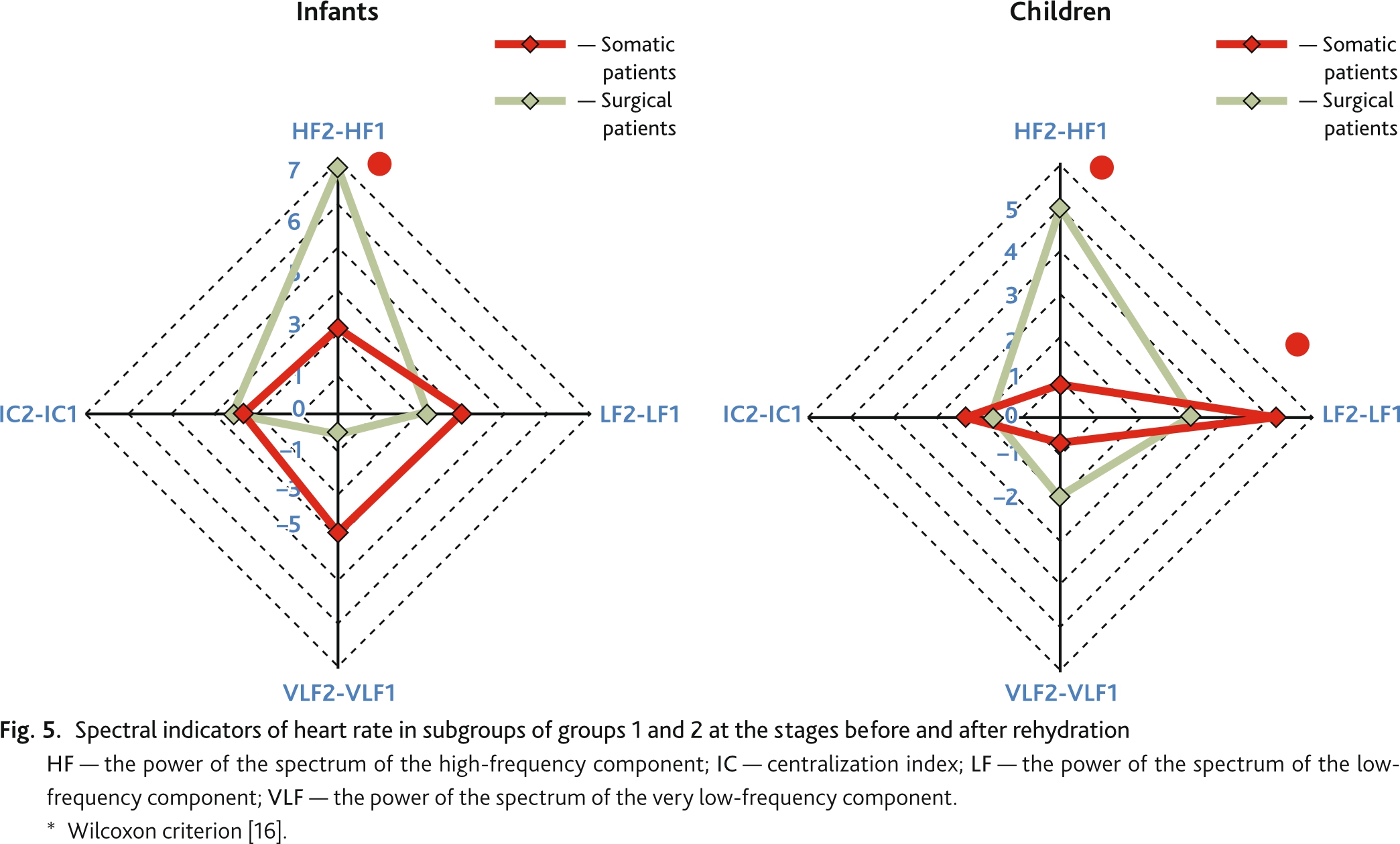
The results of intragroup comparison at the stages before-after emergency rehydration in the group of newborns revealed a sympatholytic effect of the bolus volume, but without significance (in the somatic subgroup SI1 = 532 [297; 1301] – SI2 = 537 [299; 854], p = 0.057 and in surgical subgroup SI1 = 766 [276; 1265] – SI2 = 629236 [122; 1009], p = 0.741) (Fig. 4). In the somatic subgroup, the volume of intravenous infusion determined a significant decrease in mean arterial pressure (p = 0.000). In the presence of an epidural block, the response to the infusion volume was represented by a trend towards an increase in MAP, and a significant increase in HR. Somatic newborns decreased in the HF proportion to the volume of infusion; the surgical ones had no changes. Children without EA had a significant growth of low-frequency waves, in the subgroup after surgery, the dynamics were not confirmed (Fig. 5–8).

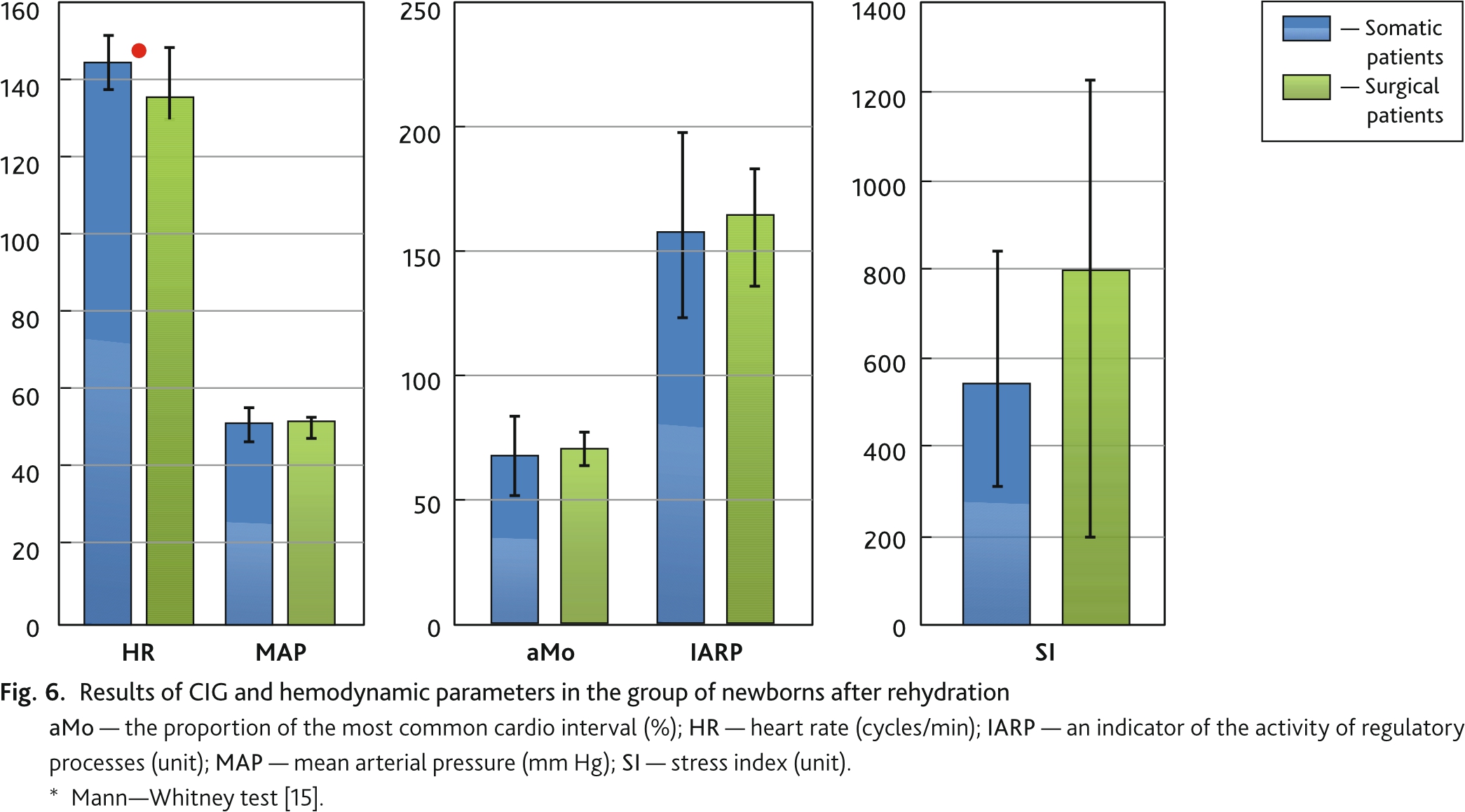
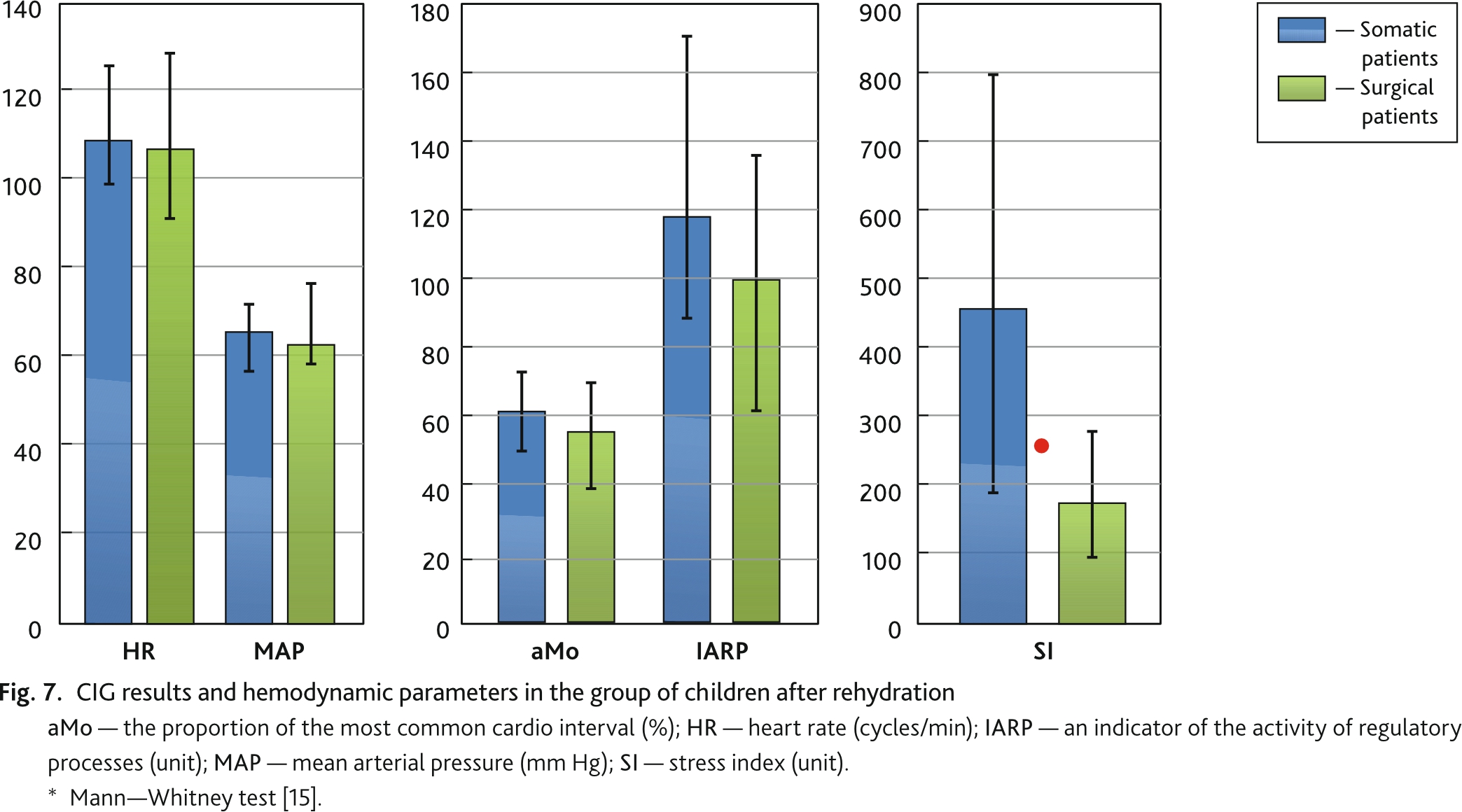
Newborns without sedation and analgesia showed a multidirectional response to bolus infusions. With a decrease in aMo and an increase in the variation range, an increase in SI was noted with the suppression of the HF of the respiratory in the absence of the heart rate response. In 62–72 % of cases in the somatic children subgroup, a direct inhibitory effect of rehydration on the adrenergic level was found, expressed in a decrease in aMo and SI (p = 0.001), vegetative balance, the indicator of the activity of regulatory processes and the vegetative rhythm indicator. The infusion bolus had an impact on the activity of the vasomotor center, indirectly reflected in the increase in the proportion of LF (p = 0.037). Volemic bolus revealed hemodynamic stability with the moderate sympathetic level with a slight decrease in indicators and indices in children postoperatively.
Newborns have the hemodynamic reconstruction of circulatory circles, the immature afferent and efferent pathways, the low receptor sensitivity, and high proportion of the extracellular water sector in the first week of life [3, 6, 7]. Their neurovegetative response to preload or afterload is unpredictable and has been studied in limited extent. Studied data showed that newborns after surgical stress have a clinical picture of a discrepancy between the stability of routine hemodynamic parameters and the level of sympathicotonia. To the results, there was a clinical discrepancy between the stability of routine hemodynamic parameters and the sympathicotonia in newborns in the postoperative period. Physiologically, this state is interpreted as a “protection reaction”, nociceptive fibers of the depressor type reflexively exert a restraining effect on the sympathetic system [14, 17, 18]. However, newborns with a predominance of cardiac adrenergic regulatory mechanisms over cholinergic ones have low myocardial sensitivity to catecholamines due to the weak development of β-adrenergic receptors. Adrenaline has no effect on the heart of the newborn, but also act paradoxically, reducing the heart rate. In newborns, reflex regulation of cardiac activity is possible, but the manifestations are weak and inconsistent [14, 19]. The cardiointervalography data and frequency analysis did not differ significantly in the two subgroups. The spectral analysis components and statistical indicators of CIG were similar in group 1. The response to the volume of infusion (stage 1–2) differed in subgroups: in newborns with regional block, it was expressed by significant tachycardia (p = 0.02) with the stability of MAP and CIG data (the Bainbridge reflex was explained by atrial stretch receptor excitation); in newborns without EA, the hemodynamic response was represented by a decrease in MAP (p = 0.000) without a chronotropic component, a decrease in the activity of the volumetric component (a significant decrease in the proportion of HF, p = 0.032). There was a sympatholytic effect (the stress index reduction) of the infusion bolus, but the significance was not confirmed (p = 0.057). There are no studies on the response of the autonomic nervous system to infusion therapy in newborns; it is not possible to compare the results obtained.
In children’s subgroups at stage 1, heart rate variability indicators differed significantly (p < 0.05). The sympathetic reactions were suppressed in children, the stress sympathicotonia was moderate, the indices were close to the balance of the autonomic nervous system (SI, IARP, aMo) in the early postoperative period. An additional bolus of hydration with the intraoperative volume did not contribute to the overstrain of autonomic regulation during general anesthesia with regional block. The redistribution of infusion therapy volumes (saline solutions) with a decrease in vascular tone was realized through the feedback of the baroreceptor system and the vasomotor center of the medulla oblongata [14, 18, 20], which clinically explained the isolated decrease in MAP (p = 0.001) only in children. In children somatic subgroup, a combination of stress factors: fear, pain, dehydration was realized through a decrease in heart rate variability switching to the stabilizing effect of the cardiovascular system centralization under overstrain. It is known that SI reflects the degree of tension of regulatory systems, and the VLF component of the spectrum characterizes the sympathetic activity of the autonomic nervous system and reflects the influence of the suprasegmental regulatory level, the cortical psycho-emotional and functional state, and is a sensitive indicator of an energy-deficient state [18, 20, 21]. Shlyka N.I. (1991), Gushturova I.V. (1994) showed the blood circulation in 6–7 year old children with central heart rate regulation was characterized by a less rest heart economical mode compared with peers under moderate autonomic regulation. Normally, vagal activity is the main component of the high-frequency component and is well reflected by the HF % indicator (the norm is 35–50 % of the total power of the spectrum [5, 20]. A decrease in this proportion in the spectrum indicates a shift in the autonomic balance towards the predominance of central regulation. In somatic subgroup, a significant high spectrum wave suppression (respiratory waves) was noted with low frequency stability. The chest negative pressure in increasing the respiratory rate or forcing the breath temporarily reduced the left heart volume, cardiac output, causing stimulation of the baroreceptors therefore [14] The emergency infusion volume had a positive sympatholytic effect. An hour after there was a shift in the CIG indices towards a decrease in the activity of the sympathetic division, the appearance of heart rate variability with low wave increase (vasomotor waves, or Mayer’s waves) (LF = 0.037). They arose due to fluctuations in baroreceptor activity [18, 20]. An increase in blood pressure excited baroreceptors, leading to inhibition of sympathetic nerve centers and a decrease in pressure after a few seconds. Suppression of baroreceptor stimulation determined the activity of the vasomotor center and an increase in blood pressure after a few seconds. The maturation of the regulation of vascular tone and the pumping function of the heart infusion therapy contributes to a more economical work of the cardiovascular system with age.
In the newborn group, heart rate variability is suppressed, hypersympathetic activity and dominance of the central circuit of heart rate regulation are not tied to nosological stratification. Rehydration therapy had a depressing effect with a decrease in volumetric regulator activity, which was regarded as an unfavorable marker of hemodynamic instability. In the neonatal period, the volume of rehydration is considered by us as a stress factor. One should be wary of the method of emergency rehydration in the intensive care of this category of patients. It is reasonable to start a tolerant assessment for infusion therapy with monitoring of the neurovegetative status and control markers that are sensitive to latent heart failure, hypervolemic status. The prospect of a B-type natriuretic peptide is proposed.
The autonomic nervous response to a bolus volume under an epidural analgesia is limited, while the peculiarities of reactions are noted: an increase in tachycardia in newborns and an increase in blood pressure in children.
Infusion therapy has a direct suppressive effect on the adrenergic level due to baroreflex volumetric stimulation in somatic children. The speed of achieving autonomic balance, recovery of heart rate variability and the search for etiopathogenetic therapy with a sympatholytic effect in older children with cardiovascular maladaptation is of interest for further research.
Disclosure. The authors declare that they have no competing interests.
Author contribution. All authors according to the ICMJE criteria participated in the development of the concept of the article, obtaining and analyzing factual data, writing and editing the text of the article, checking and approving the text of the article.
Ethics approval. This study was approved by the local Ethical Committee of Novosibirsk State Regional Clinical Hospital, Novosibirsk, Russia (reference number: 1-09.03.2021).