
Children's need for parental presence is important both in everyday life and especially when a child faces a critical situation [1–3]. When a child is in the intensive care unit (ICU), it is vital to use all possible resources to restore the child's well-being and health [3, 4]. At the same time, parents being beside the child are one of the best resources for their child's health care [5, 6]. In addition, parents present with their children in ICU, as well as their children, have reduced stress, anxiety and fear, and uncertainty [7].
The care of a child in ICU by medical staff, who make a child the centre of their attention and care within a family-oriented approach, is established from the perspective of recognising the patient as an individual and part of his/her family [8], respecting his/her needs and, in particular, the need for a parent or other loved one beside him/her at any time [4, 9], as well as his/her right to make own decisions [10].
However, medical staff often restricts or does not allow parents to be present in the intensive care unit [11, 12]. The excessive anxiety parents may experience when they are in ICU with their child and the fear of what their child experiences are thought to be among the reasons for separating them [13, 14]. There is an opinion among healthcare professionals that parents can influence their decision-making in professional activities [13]. They emphasize a point of lacking staff, space and/or time needed to give adequate attention to the patient's parents [15]. The reason for the parents' refusal to be with the child in a critical situation may also be the fact that medical staff has no enough experience of such situations [13, 16].
However, several studies show that presence of parents together with physicians and nurses when dealing with their child's critical situation leads to increased mutual confidence, decreased anxiety, and greater involvement of parents in such situations in future [1, 14]. For medical staff and parents, this creates the assurance that everything possible to help the child has been done, nothing vital has been lost, and moral standards have been respected [14].
Motivation for implementation of this study was as follows: in the practice of national health care, such aspects were not studied; and the role and significance of joint stay of parents with their children in ICU was never evaluated from the position of medical personnel working there.
Objective: To evaluate social and psycho-emotional aspects of joint stay of a family member (parents) with a patient (child) in ICU from the viewpoint of the medical stuff.
Hospitals that declared following the principles of a family centered care (FCC) approach in treatment of patients were involved in the study. The duration of adherence to the family-centred approach in the treatment of patients as judged by the healthcare providers themselves was 1 year and more than 10 years — 4.00 (2.00; 10.00) years. The health care institutions included in the study were level 2 and 3 in the national health care system. Median of bed capacity count in these institutions was 448, of which 7.5 (median) beds accounted for the intensive care unit (Table 1).
Table 1. Characteristics of medical institutions
| No. | Constituent of the Russian Federation | Medical institution | Level of the medical institution in the RF healthcare system | Total bed capacity of medical institution | ICU bed capacity of the medical institution that participated in the study |
|---|---|---|---|---|---|
| 1 | Artyom, Primorsky Krai | Regional State-Funded Medical Institution “Artemovskaya Children's Hospital” | 2 | 105 | 5 |
| 2 | Izhevsk | Republican Children's Clinical Hospital of the Udmurt Republic | 3 | 638 | 18 |
| 3 | Kaliningrad | Federal State-Funded Medical Institution “Regional Children’s Hospital of the Kaliningrad Region” | 3 | 387 | 9 |
| 4 | Kazan | State Autonomous Medical Institution “Republican Children's Clinical Hospital of the Ministry of Health of the Republic of Tatarstan” | 3 | 923 | 27 |
| 5 | Petrozavodsk | Federal State-Funded Medical Institution of the Republic of Karelia “Republican Children’s Hospital” | 3 | 320 | 6 |
| 6 | Tambov | Federal State-Funded Medical Institution “Tambov Regional Children's Clinical Hospital” | 3 | 509 | 6 |
| 7 | Tyumen | Federal State-Funded Medical Institution of the Tyumen Region “Regional Children's Clinical Hospital No. 2” | 3 | 925 | 73 |
| 8 | Khabarovsk | Regional State-Funded Medical Institution “A.K. Piotrovich Regional Children’s Clinical Hospital” | 3 | 344 | 6 |
Evaluation of studies indicators was carried out using the questionnaires for the following periods: I — (01.11.2020 — 31.12.2020), II — (01.01.2021 — 28.02.2021), III — (01.03.2021 — 30.04.2021), IV — (01.05.2021 — 30.06.2021).
Questionnaire design was arranged in such a way that the respondent could choose one of the answers most appropriate in his/her opinion from several proposed answers to the question. “Unsatisfactory” and “satisfactory” ratings were considered low, they corresponded to the level lower than the level respondent sets for this indicator according to his/her moral certainty. Accordingly, “good” and “very good” ratings were considered high, and they corresponded to the target level that respondent sets for this indicator according to his/her moral certainty. The total number of completed and analysed questionnaires was 417. Questionnaires with incomplete correspondence with inclusion criteria or incorrect data entered were not included in the statistical analysis.
Medical staff completed the questionnaires anonymously during their off-duty hours. Respondents signed an informed consent form that included information about the research, confidentiality rules and the contact details of the independent research expert. After respondents signed informed consent, the expert provided a questionnaire for filling in. Respondents could choose when and where to fill in the questionnaire and how to submit it to the expert in an anonymous manner.
Positive opinion No. 3 dated 20.08.2020 on the study conduction was obtained within the decision of the local ethical committee (LC) of the Children’s Palliative Care Foundation, Moscow.
The obtained data were subjected to descriptive analysis with estimation of median and quartile span values — Me (Q1; Q3), mean and standard deviation values — M ± σ, as well as share of the indicator both in quantitative and percentage terms.
In the survey, the opinion of doctors (intensivists) was formed based on the analysis of 158 questionnaires received from 8 cities (Artyom, Izhevsk, Kazan, Kaliningrad, Petrozavodsk, Tambov, Tyumen, Khabarovsk) of the total number of participants in the study (in Appendix Table П1 of the online version of the article).
When assessing their satisfaction with ICU location within the medical institution and its floorspace capacity (1.2), 17.3 % of respondents reported Unsatisfactory and 19.2 % reported Satisfactory, despite the Good global rating — 4.00 (3.00; 4.00). In addition, more than 30 % of answers with the rating not better than Satisfactory were in the characteristics of ICU premises number and purpose of function, availability of consumables for diagnostic, therapeutic, sanitation and housekeeping needs, medicines, and professional technical staff in ICU (2.2–6.2, 9.2). Among doctors, Good and Very Good ratings in their answers about availability of ICU professional doctors made 62.8 % and 20.5 %, respectively; and as for availability of nursing personnel, the respective ratings were 50.6 % and 20.5 % (7.2, 8.2).
Characteristics of doctors (14.2) and nursing personnel (15.2) salary was considered Satisfactory 3 (3; 4) and 3 (2; 3), respectively, i.e., lower than expected.
Doctors evaluated their own (18.2, 19.2) and nursing staff (20.2, 21.2) professional level with predominant Good and Very Good rates 4 (4; 4) — 4 (4; 5).
ICU physicians evaluated general cultural and educational level of patient family members they had to contact as Satisfactory — 3 (2; 4); with 22.9 % of respondents were not sure about this question (22.2), and 12.4 % evaluated general cultural and educational level of patient family members as Unsatisfactory. Doctors also rated the level of patient (23.2) — 3 (2; 4) and patient representatives (24.2) — 3 (2; 4) awareness in his/her health status as low.
Doctors rated parents (parents, etc.) participation in the care of patient in ICU as Good — 4 (3; 4). The respondents rated level as Good 42.2 % and Very Good 14.9 % respectively.
Doctors, in most cases, among relatives who were with children in the ICU, indicated the mother (35 %), then the father (20 %), grandmother (17 %) and guardians (15 %) (Fig. 1), and the time spent by the parents with a patient to care for him during the day (27.2) was 12 hours in most cases 12 (1; 24).
Fig. 1. The patient's representative visiting and caring patient in the ICU according to the survey of physicians (in Appendix Table П1)
Physicians evaluated the kind of assistance provided by family members to a patient (30.2) in ICU, and 89 % reported sanitary and hygienic care (30.2a), 82 % — feeding (30.2b), 32 % — assistance to medical staff in patient transportation and dislodging (30.2e). In addition, physicians noted participation of parents in decision-making on diagnostic and treatment measures/interventions for the patient as 15 % (30.2g), and in searching for and provision of medicines and equipment necessary for the patient in ICU as 8 % (30.2h).
Doctors rated the level of preparation of parents to caring for a patient at the stage of his admission to ICU (31.2) as Satisfactory 3 (2; 3), and in patient transition from ICU (32.2) as Good — 4 (3; 4).
According to doctors, claims from patients and their family members, which are mentioned in the questionnaire, were mostly due to their underestimation of the complexity of the situation with the patient — 58 % (33.2а), personalities of the patients — 33 % (33.2b) and their parents — 48 % (33.2c). In the total list of complaints, level of comfort in ICU and medical institution, as perceived by doctors, accounted for 5 % (33.2g, 33.2h).
In the responses to the question about innovations introduced into ICU work at the suggestion of the patient family members, doctors most often referred to the format of receiving patient information 33 % (34.2a), management of admission and stay with the patient in ICU ward — 25 % (34.2b), patient representative participation in care of the patient in ICU — 19 % (34.2c), management and format of patient representative training in care for him/her in ICU — 16 % (34.2d), management and format of medical and psychological support to patient representatives during their stay in ICU — 14 % (34.2e).
Evaluation of the survey of nursing staff (nurses) was based on the analysis of 259 questionnaires received from 8 cities (Artyom, Izhevsk, Kazan, Kaliningrad, Petrozavodsk, Tambov, Tyumen, Khabarovsk) from the total number of participants (in Appendix Table П2 of the online version of the article).
When assessing their satisfaction with ICU location within the medical institution and its floorspace capacity (1.3), 6.2 % of respondents were not sure about their answer, 12.4 % reported it Unsatisfactory and 31.8 % — Satisfactory, with the Satisfactory global rating — 3.00 (3.00; 4.00). This rating was lower than those given by doctors (1.2) — 4.00 (3.00; 4.00). 50.8 % of nurses rated number and functionality of rooms in ICU (2.3), availability of consumables for diagnostic, therapeutic, sanitation, and housekeeping needs in ICU (4.3, 5.3) not higher than Satisfactory. Doctors rated the same positions as Good (in Appendix Table П1). Nurses considered equipment/devices (3.3), medicines (6.3), professional doctors (7.3), professional nursing staff (8.3), professional technical staff (9.3) availability in ICU to be Good — 4 (3; 4). Over 70 % of doctors, when asked about the availability of doctors and nurses in ICU, rated it Good and Very Good (7.2, 8.2, in Appendix Table П1).
Nurses reported the rating of their own salary level (14.3) as Satisfactory 3 (2; 3) and doctors rated their own salaries (15.3) below Satisfactory 2 (1; 3). It should be noted that 48.2 % of responding doctors choose the answer “Not Sure”.
Nursing staff rated their own professional level (20.3, 21.3) and doctor professional level (18.3, 19.3) as Good 4 (4; 5) — 4 (4; 5).
ICU specialists evaluated general cultural and educational level of patient family members the nurses had to contact (22.3) as Satisfactory in general — 3 (1; 3). Among those surveyed, 29.5 % were not sure answering the question, 9.2 % rated it as Unsatisfactory, and 37.1 % as Satisfactory. Respondents also rated the level of patient (23.3) — 3 (2; 4) and patient representatives (24.3) — 3 (2; 4) awareness in his/her health status as low.
Nursing staff (25.3) rated participation of parents (family members) in care of a patient in ICU as Satisfactory 3 (3; 4). This was different from the Good rating 4 (3; 4) reported by the doctors (25.2). Nurses defined the level of "unsatisfactory" and "satisfactory", respectively, by 15.7 % and 39.8 % of respondents.
According to nurses, among relatives who were with children in the ICU, there were mother (29 %), father (20 %), grandmother (19 %) and grandfather (5 %) (Fig. 2), and parents stayed in ICU with their child (patient) to care for him (27.3) for 6 hours 6 (1; 24) a day, and this was different from answers of the doctors — 12 (1; 24).
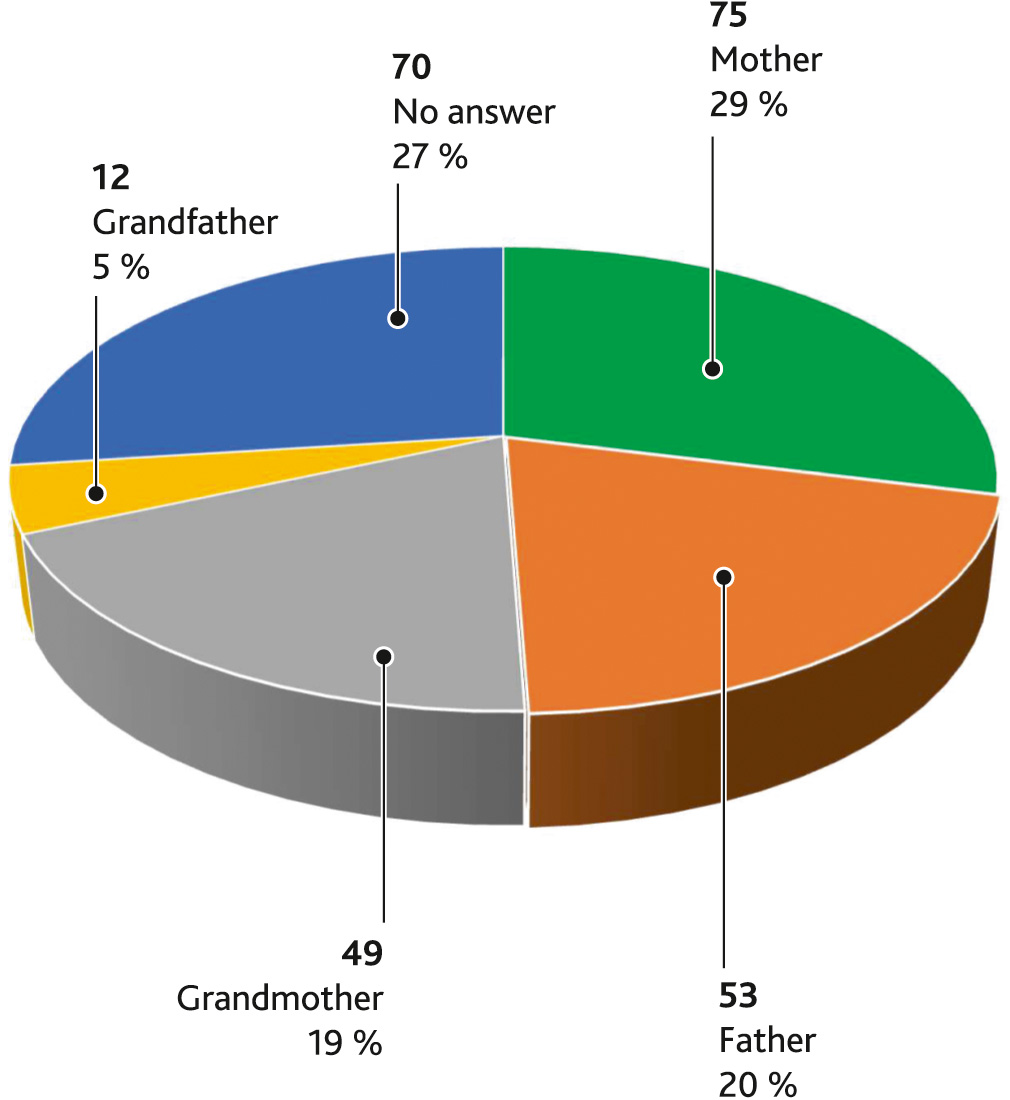
Fig. 2. The patient's representative visiting and caring him in the ICU according to the survey of nurses (in Appendix Table П2)
Nursing staff evaluated the kind of assistance provided by family members to a patient (30.3) in ICU, and 91.5 % reported sanitary and hygienic care (30.3a), 81.9 % — feeding (30.3b), 47.1 % — assistance to medical staff in patient transportation and dislodging (30.3e). 28.2 % of respondents reported that parents were involved in watching monitors and other devices connected to the patient (30.3c); 26.3 % reported assistance to nursing staff in implementation of treatment protocol prescribed by doctor to the patient (30.3d); and 10 % reported assistance in searching for and provision of medicines and equipment necessary for the patient in ICU (30.3h).
Nurses rated the level of preparation of parents to caring for a patient at the stage of his admission to ICU (31.3) and in patient transition from ICU (32.3) was the same — Satisfactory 3 (2; 3) and 3 (3; 4), respectively. However, at the stage of patient admission to ICU nurses reported about 32.7 % of Unsatisfactory skills and knowledge of parents in caring for their child, and only in 13.5 % were Good; but after transition to the specialized unit these ratings change to 11.2 % of Unsatisfactory and 43.9 % of Good.
According to nursing staff, claims from patients and their family members, which are mentioned in the questionnaire, were in the most instances due to their underestimation of the complexity of the situation with the patient 48.6 % (33.3а), personalities of the patients — 36.3 % (33.3b) and their parents — 39.8 % (33.3c), and low awareness of the patient’s health 23.2 % (33.3f). In the total list of complaints related to comfort level in ICU and medical institution, the nurses results were 11.2 % и 4.2 %, respectively (33.3g, 33.3h), while the doctors result it is within 5 % (33.2g, 33.2h).
In the responses to the question about innovations introduced into ICU work at the suggestion of the patient family members, nurses most often referred to the format of receiving patient information 17.8 % (34.3a), management of admission and stay with the patient in ICU ward — 28.6 % (34.3b), patient representative participation in care of the patient in ICU — 24.3 % (34.3c), management and format of patient representative training in care for him/her in ICU — 22.8 % (34.3d), management and format of medical and psychological support to patient representatives during their stay in ICU — 18.1 % (34.3e).
According to the survey of doctors and nurses in general, adherence to family-centered approaches in the care of children in ICU was positive. In particular, despite the rather low rating of working conditions in terms of premises used and logistics, salary level, which are potentially negative factors in attitudes to the additional workload from parents staying with children, most of the responding healthcare professionals surveyed noted the positive aspects of interaction with relatives of patients. In observational study by Mattson J. et al. (2013), it is noted that nurses in their work primarily focus on health status of a child; and at the same time, quality and scope of child care provided by nurses can be unsatisfactory [18]. In our study, we received favourable opinions from both doctors and nurses about participation of parents in care of their children in ICU and improving their skills and knowledge in caring for their child. This is undoubtedly of significant importance, as Dudley N. et al. (2015) indicated in their study; they make a point that parents can interpret child’s signals and facilitate communications between medical staff and children. When parents are not involved in the care of the child, his/her signals may be misinterpreted or completely missed by medical staff [6]. The essential role of parents in achieving quality care for a sick child has also been highlighted in other works describing how healthcare staff with previous experience of parents participation is more positive about involving parents in the care of their children [1, 14]. Among the complaints from parents and patients medical staff had to face, both doctors and nurses in most cases mentioned a lack of underestimation of the complexity of the situation with the patient, personalities of patients and their relatives, which may to some extent be the result of insufficient attention of medical staff to them and failure to fully and clearly convey the required information. This may be indicative of the fact that it is necessary to train and practice medical staff in dealing with parents in critical situations, develop and implement algorithms of behaving and communicating with patients staying in ICU and their relatives [18].
The Family-Centered Approach of keeping parents with their children in Intensive Care Unit does not add considerable moral and work load to professional activities of medical staff in these units; on the contrary, this creates favourable conditions for improving the knowledge and skills of parents in caring for their children and assisting the ward staff. Further research is needed on this issue to identify current practices and trends within the scope of ICU care, and to develop and implement new algorithms for the interaction of healthcare staff with patients and family members to improve quality and efficiency of medical care.
Data availability. Appendices available here.
Funding. The research was carried out with the support of the Presidential Grants Fund of the Russia Federation, Grant No 20-2-006267 dated 08.07.2020.
Disclosure. The authors declare that they have no competing interests.
Author contribution. All authors according to the ICMJE criteria participated in the development of the concept of the article, obtaining and analyzing factual data, writing and editing the text of the article, checking and approving the text of the article.
Ethics approval. This study was approved by the local Ethical Committee of Council of the Charitable Foundation for the Development of Palliative Care “Children’s Palliative”, Moscow, Russia (reference number: 3-20.08.2020).